Introduction
Rupture of the tendon of the popliteus muscle (TP) is usually secondary to trauma in forced varus with flexion or forced external rotation of the knee(1). Isolated injury is rare, and the lesion usually occurs in the context of other meniscal or ligamentous lesions(2,3).
The range of TP injuries can take place at the muscle-tendon junction or secondary to avulsion at the point of insertion in the external femoral condyle(3). The initial diagnosis is usually difficult to establish, since the physical examination reveals only very subtle and scantly specific findings(4,5). Altered gait with great patient apprehensiveness should cause us to suspect the injury, though complementary tests are essential in order to confirm the diagnosis.
We present the unusual case of a woman with osteochondral fracture of the external femoral condyle affecting the insertion of the TP, and causing episodes of joint subluxation with pain and instability sensation upon walking. Surgical treatment was decided in view of the ineffectiveness of initial conservative treatment and persistence of the instability symptoms.
Clinical case
A 30-year-old woman reported to the emergency room due to pain and functional impairment following indirect low-energy trauma of the left knee. The physical examination revealed signs of local inflammation, pain in response to palpation of the lateral joint line, and painful functional limitation in both active and passive mobilization that made walking impossible.
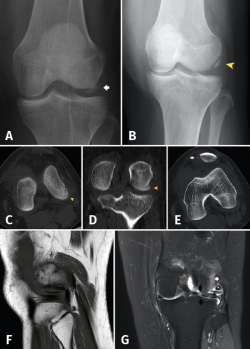
The initial radiographs revealed fracture of the external femoral condyle with an osteochondral fragment lodged in the lateral femorotibial joint space (Figure 1A). This displacement was not confirmed at radiological controls following immobilization (Figure 1B). Computed axial tomography (CAT) revealed a non-displaced double fracture line at the posterior margin of the external femoral condyle, parallel to the joint surface of the latter and measuring 21 mm in length, together with signs of avulsion fracture at the medial margin of the patella, with lateral subluxation (Figure 1B).
Based on the absence of joint instability and the CAT findings, and with the suspicion of a first episode of traumatic lateral patellar luxation, orthopedic treatment was prescribed initially with a plaster cast for three weeks and followed by orthosis to allow progressive walking with the aid of crutches.
At reassessment after 12 weeks, the patient reported "joint laxity" and "failing" of the knee. The physical examination revealed altered gait with great patient apprehensiveness and a tendency towards a "varus drive" pattern, overjet in the lateral femorotibial compartment with mild laxity +/+++ in varus and 0 and 30 degrees of flexion, together with an inconclusive dial test. The Lachman and anterior and posterior drawer in neutral rotation manoeuvres proved negative. The posterolateral rotary drawer test showed subtle asymmetry, with a joint balance of 0 at 115 degrees. The MRI study revealed a subchondral lesion in the loading zone of the external femoral condyle accompanied by intense bone edema and joint effusion. The external meniscus presented a pseudo-discoid appearance with suspected rupture (Figure 1C-D).
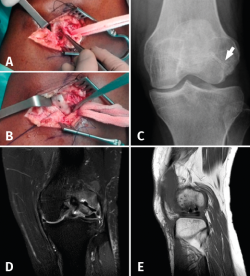
In view of the poor clinical course over follow-up and the MRI findings, surgery was indicated. Two procedures were carried out in the same surgical step. A first arthroscopic evaluation confirmed the presence of the osteochondral fracture measuring 21 mm in length, with involvement of the insertion of the tendon of the popliteus muscle, and incomplete lateral discoid meniscus rupture requiring partial meniscectomy. Partial damage to the anterior cruciate ligament (ACL) was also observed, affecting less than 50% of the ligament; no treatment was therefore required. The second procedure involved open surgery with a guided miniarthrotomy (Figure 2A) that confirmed preservation of the external lateral ligament and anterior luxation of the TP adhered to the fragment. In this procedure peripheral suturing was made entirely within the external meniscus; roughening and osteosynthesis of the fragment was performed with two 2.7 mm cannulated magnesium alloy screws measuring 20 and 24 mm in length to affix the fragment and restore the original position of the TP (Figure 2B-C).
During the postoperative period the knee was immobilized in extension for 48 hours, followed by the start of flexion-extension exercises and postponing the rehabilitation program until the second week after surgery. A stabilizing knee guard was fitted to gradually increase the mobility range, and assisted weight bearing was allowed in the fourth week. Flexion was limited to 90 degrees in the first 6 weeks. Withdrawal of the crutches started after 8 weeks, with removal of the orthosis after 12 weeks.
After 15 months of follow-up, the patient was asymptomatic, the joint failure episodes had disappeared, and she had returned her daily activities - though she had not resumed sports activities. In the first few months the control radiographs showed a radiolucent area around the implants - these being common and non-pathological radiological signs. The control MRI scan after four months evidenced integration of the osteochondral fragment of the external femoral condyle (Figure 2D-E).
Discussion
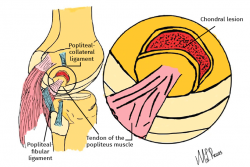
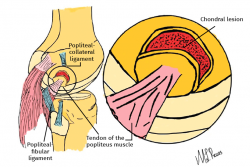
The main elements of the posterolateral complex (PLC) of the knee are the lateral collateral ligament, the TP and the popliteal-fibular ligament (Figure 3). Its principal function is knee varus stabilization and limitation of posterior displacement and external rotation of the tibia(1).
The TP is one of the main components of the PLC. The popliteus muscle originates from a powerful tendon measuring about 2.5 cm in length within the depression in the anterior zone of the sulcus in the lateral femoral condyle(2). The TP, covered by the synovial membrane, forms a thin and flat triangular-shaped muscle that inserts in the two medial thirds of the triangular surface proximal to the popliteal line in the posterior surface of the tibia(2). The tendon is also joined to the arcuate ligament and, according to Last(3), up to half of its fibres insert in the lateral meniscus. The function of the popliteus muscle is subject to controversy, though it may act in conjunction with the meniscofemoral ligaments (Humphry and Wrisberg) to control movement of the lateral meniscus on flexing the knee(2). There is a close association between TP injury and damage to the anterior and posterior cruciate ligaments(2,6).
The mechanism of TP injury is not clear. The muscle may be damaged by direct high-energy external trauma combined with forced external rotation of the partially flexed knee or the application of varusising force(2).
Isolated injury of the TP may occur within the muscle body, at the muscle-tendon junction, or secondary to avulsion of an osteochondral fracture that includes its insertion(7). Its clinical presentation has also been described associated to or resulting from osteochondritis dissecans, with displacement of the fragment as a result of traction exerted by the tendon itself(6).
The treatment of isolated injuries of the TP has not been well established, and different treatments have been described in the literature. Some authors have chosen to repair the insertion of the tendon, while others advocate a conservative approach(4,10). Westrich et al.(8) published a case of TP avulsion that was affixed using sutures, with a good functional outcome. Mirkopulos et al.(4) likewise reported a case of isolated TP avulsion without joint instability, performing open repair with a metal screw and washer. Following repair, the patient remained asymptomatic and returned to his previous activities after 18 months of follow-up. Grue(10) in turn published a case of isolated TP avulsion that was subjected to conservative treatment, allowing the patient to resume daily activities.
There is no consensus regarding the best treatment option for isolated TP avulsion. Long-term studies with a larger number of patients are therefore needed to define the most adequate treatment(9).
Different types of fixation can be used in surgical treatment to stabilize the osteochondral fragments, depending on the preference of the surgeon. A novel strategy is the use of bioabsorbable compression screws made of a magnesium alloy(11). In contrast to metal screws, these screws do not need to be removed and moreover offer the advantage of low interference in MRI imaging. We therefore consider their use to be very interesting.
In our case, the scantly specific findings of the initial physical examination and the CAT data, evidencing no displacement of the fracture, caused us to wrongly orientate the treatment strategy - minimizing the diagnosis to an episode of patellar instability. A guided physical examination, in which gait inspection proved crucial, together with the MRI images, allowed us to establish the definitive diagnosis of this rare condition.
If this type of injury goes unnoticed and is not treated on time, it may cause functional limitation, with gait problems, and thus adversely affect patient quality of life.
Conclusions
Isolated TP avulsion injuries are rare. The clinical diagnosis is difficult to establish, since the physical examination reveals only very subtle and scantly specific clinical findings. Analysis of the gait pattern is crucial, and MRI is the imaging technique of choice. Magnesium alloy screws are an alternative to be taken into account thanks to the stability they afford and because they may avoid the need for second surgery.