Evolution of the indication of arthroscopic treatment for femoroacetabular impingement and of the indication of total hip arthroplasty in patients under 60 years of age
Evolución de la indicación del tratamiento artroscópico del pinzamiento femoroacetabular y de la indicación de la artroplastia total de cadera en menores de 60 años
Resumen:
Objetivo: comparar las prescripciones de la cirugía artroscópica de cadera para el diagnóstico de pinzamiento femoroacetabular (PFA) y los de la artroplastia total de cadera (ATC) para un diagnóstico de coxartrosis primaria o idiopática.
Métodos: estudio observacional, transversal y retrospectivo, realizado en un solo centro, hospital terciario del Sistema Nacional de Salud, entre 2009 y 2015. Se analizó el número total de inclusiones en lista de espera para ambos procesos, artroscopia de cadera para PFA y ATC para coxartrosis primaria o idiopática durante el periodo de estudio, en pacientes menores de 60 años.
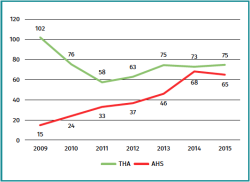
Resultados: se cuantificó el número de inclusiones en lista de espera para ambos procedimientos, totalizando 810 (100%) pacientes: 288 (35,6%) correspondieron a artroscopia de cadera por diagnóstico de PFA y 522 (64,4%) correspondieron a ATC por un diagnóstico de coxartrosis. Se observó un incremento del 433,3% de la artroscopia de cadera por PFA y una disminución de la incidencia de prescripción de ATC primaria de un 26,5%. Observamos que, a medida que aumentaban las prescripciones de artroscopia de cadera, las prescripciones de ATC disminuían. Los procedimientos casi alcanzan la paridad en 2014.
Conclusiones: en nuestro centro, ha habido un aumento significativo en el uso de la técnica artroscópica de cadera para el tratamiento de la PFA. Según estos resultados, en nuestro centro, se ha observado una mayor prescripción de la cirugía de conservación de cadera en sujetos menores de 60 años mediante artroscopia y una disminución de la prescripción de artroplastia total de cadera, aunque no se puede establecer una relación causa-efecto.
Nivel de evidencia: nivel 3.
Relevancia clínica: al igual que en otros centros, ha habido un aumento significativo en el uso de la técnica artroscópica de cadera para el tratamiento de la PFA. En el periodo de estudio, en nuestro centro, se ha observado una mayor prescripción de la cirugía de conservación de cadera en sujetos menores de 60 años mediante artroscopia y una disminución de la prescripción de artroplastia total de cadera, aunque no se puede establecer una relación causa-efecto.
Abstract:
Objective: to compare the indications of arthroscopic hip surgery for the diagnosis of femoroacetabular impingement (FAI) and of total hip arthroplasty (THA) for the diagnosis of primary or idiopathic coxarthrosis.
Methods: a retrospective, cross-sectional, single-centre observational study was carried out in a tertiary hospital of the Spanish public healthcare system between 2009 and 2015. An analysis was made of the total number of inclusions on the waiting list for both procedures — hip arthroscopy for FAI and THA — for primary or idiopathic coxarthrosis during the study period, in patients under 60 years of age.
Results: the number of inclusions on the waiting list for both procedures was 810 (100%) patients: 288 (35.6%) corresponded to hip arthroscopy due to the diagnosis of FAI and 522 (64.4%) corresponded to THA due to a diagnosis of coxarthrosis. An increase of 433.3% was observed in hip arthroscopy due to FAI, with a 26.5% decrease in the incidence of the indication of primary THA. The indications referred to THA were seen to decrease as the indications of hip arthroscopy increased. The two procedures were almost equalised in 2014.
Conclusions: there has been a significant increase in the use of hip arthroscopy for the treatment of FAI at our centre. Based on these results, we have observed an increase in the indication of conservative arthroscopic hip surgery in individuals under 60 years of age at our centre, together with a decrease in the indication of THA, though no cause-effect relationship can be established.
Level of evidence: level 3.
Clinical relevance: as at other centres, there has been a significant increase in the use of hip arthroscopy for the treatment of FAI. During the study period, there has been an increase in the indication of conservative arthroscopic hip surgery in individuals under 60 years of age at our centre, together with a decrease in the indication of THA, though no cause-effect relationship can be established.
Introduction
Hip osteoarthritis or coxarthrosis is very disabling in its advanced stages(1,2). The underlying cause of coxarthrosis has not been fully established. However, in 2003, Ganz et al. described femoroacetabular impingement (FAI) as one of the factors predisposing to coxarthrosis(3).
Femoroacetabular impingement is a disease condition resulting from a pincer-type morphology of the acetabulum or from a cam-type morphology of the femoral head and neck. This, combined with specific kinematics, produces biomechanical alterations that lead to coxarthrosis(4,5,6). Although a logical relationship has been established between FAI and coxarthrosis, particularly in cam-type lesions, this is not always so. Likewise, from the clinical perspective, some patients with FAI-type anatomical alterations in the imaging studies are seen to be asymptomatic(7). The development of arthroscopic techniques in general and research into the association between FAI and coxarthrosis have favoured the use of hip-preserving surgical procedures such as arthroscopy(8).
At present, arthroscopic hip surgery (AHS) is commonly performed in departments of orthopaedic surgery(9). Hip arthroscopy has been shown to adequately correct FAI, with few complications and relatively short recovery periods, and is seen to afford very satisfactory outcomes over the short and middle term(10,11,12,13,14). In view of the notion that FAI predisposes to coxarthrosis, and as a result of improved understanding of the syndrome, the number of patients diagnosed with FAI and the number of hip arthroscopies have increased rapidly in the last few decades(15,16). In our Department, the hip surgeons have been performing AHS for over 10 years. The present study was thus carried out to compare the evolution over time of the indications of AHS referred to the diagnosis of FAI and the evolution of the number of indications of total hip arthroplasty (THA) referred to a diagnosis of primary or idiopathic coxarthrosis in patients under 60 years of age. The study hypothesis was that in this time period, with the incorporation of AHS, the number of indications of THA has decreased.
Material and methods
A retrospective, longitudinal, single-centre observational study was carried out. The trial was conducted in the Department of Orthopaedic Surgery and Traumatology of a tertiary hospital of the Spanish public healthcare system between January 2009 and December 2015. The patients were identified from our orthopaedic surgery registry. The study was evaluated and approved by the Ethics Committee with reference 2016_25 (ARTROS2016). The inclusion and exclusion criteria were evaluated based on the information contained in the electronic health records system.
The patients were included in the statistical analysis if they met all the following inclusion criteria: 1) patients between 18-60 years of age at the time of surgery; and 2) patients subjected to elective hip surgery during the period between January 2009 and December 2015 due to FAI (International Classification of Diseases - Ninth Revision [ICD-9] code: 718.85) or primary or idiopathic coxarthrosis (ICD-9: 715.9). A review was made of the surgical waiting list and of the surgical sheets of all the patients between 18-60 years of age (1260 surgeries) in order to identify individuals operated upon by the Hip Unit of our Department, with FAI and coxarthrosis, subjected to surgery with other codes, or who had been wrongly coded. The exclusion criteria were: 1) patients subjected to primary hip arthroscopy for other reasons, such as diagnostic arthroscopy, intraarticular free bodies, etc.; 2) patients subjected to THA for other reasons such as prosthetic revision surgery, fractures, avascular necrosis, etc.; and 3) patients presenting an incomplete case history, with a missing surgical sheet (7 patients).
Statistical analysis
Categorical variables were reported as absolute frequencies and percentages. Quantitative variables were reported using measures of central tendency: mean, median and standard deviation (SD). The trend in the number of both surgeries during the follow-up period (7 years) was evaluated using the Pearson correlation coefficient with the corresponding 95% confidence interval (p < 0.05). The statistical analysis was performed using the Stata version 23.0 package (StataCorp, Texas, USA).
Results
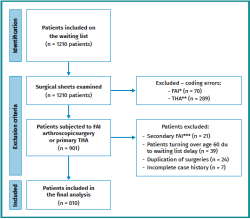
Of the 1260 reviewed surgeries, 5.6% (70 patients) presented coding errors, i.e. they corresponded to other diagnoses that had been wrongly coded as FAI. Likewise, 22.9% surgeries (289 patients) presented other diagnoses that had been erroneously coded as primary THA.
reacae.29377.fs2106020en-figure1.png
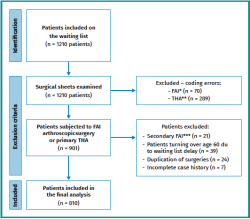
Figure 1. Flowchart showing the number of patients excluded from the final analysis of the study.
* Patients coded as presenting femoroacetabular impingement (FAI) that were operated upon for other diagnoses (diagnostic arthroscopy, intraarticular free bodies, trochanteric bursitis, snapping hip), or who underwent other procedures: diagnostic infiltrations, etc.; ** patients coded as undergoing primary total hip arthroplasty (THA) that were operated upon for other diagnoses, such as THA revision surgery, secondary coxarthrosis, proximal femoral fracture, avascular necrosis, etc.; *** FAI secondary to: epiphysiolysis, Legg-Calvé-Perthes disease, dysplasia, fracture, traumatism, osteonecrosis or infections.
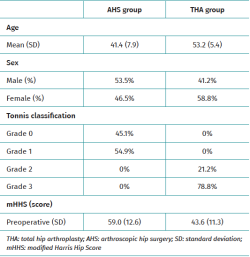
In the period between January 2009 and December 2015, the surgical waiting list reviewed by means of the surgical sheets included 810 patients subjected to AHS due to FAI and primary THA secondary to primary or idiopathic coxarthrosis between 18-60 years of age (Figure 1). Of this total, 288 patients corresponded to AHS due to FAI (35.6%) and 522 to THA secondary to primary or idiopathic coxarthrosis (64.4%). Table 1 shows the demographic data of both groups.
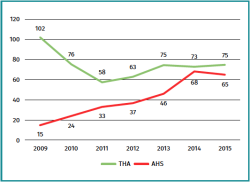
An increase of 433.3% was observed in the number of AHS due to FAI between 2009 and 2015, while the indication of primary THA decreased 26.5% in the same time period, in patients under 60 years of age (Figure 2). The indications referred to THA decreased as the indications of AHS increased, almost becoming equal in 2014. The AHS cohort showed a significant increasing trend, while the THA cohort showed a significant decreasing trend in the number of procedures performed during the mentioned 7-year period (p < 0.001).
Discussion
The main finding of the present study was that the increase in indications of hip arthroscopy due to FAI was associated to a decrease in the indications of primary THA, with a clear change in the trend in patients under 60 years of age. The two procedures were almost equalised in 2014.
We observed a tendency towards increased indication of hip arthroscopy due to FAI between 2009 and 2015. A 433.3% increment was recorded between 2009 and 2015. This tendency to increase has also been seen in other studies(16,17). Montgomery et al. reported a 365% increase in the hip arthroscopy rate between 2004 and 2009 in their cohort of patients in the United States. Zusmanovich et al. in turn found the incidence of hip arthroscopy in patients with FAI syndrome and disease of the labrum to increase 85% in the period 2011-2018 in the United States(17).
Likewise, a decrease in the incidence of primary THA of 26.5% was observed between 2009 and 2015. These data indicate a rising trend in hip arthroscopic treatment as a management approach to patients under 60 years of age with coxalgia and the absence of advanced joint degeneration (Tonnis grades I-II). From this same perspective, hip joint preservation surgery, i.e. surgery seeking to delay or avoid the appearance of hip arthrosis, has experienced an increase in the last decade(1,2,18,19,20). This is reflected in the change in trend at our centre, with hip arthroscopy being the treatment of choice for patients with FAI.
The increase in hip arthroscopy is probably due to a number of factors. These factors include surgical technical advances, improved diagnostic techniques, the expansion of indications, and increased emphasis on hip arthroscopy in resident training programmes and training scholarships(15,16,17). It has not yet been established whether this increase in hip arthroscopy results in a decrease in the number of hip prosthetic implants, however. Kowlaczuk et al., in a systematic review, concluded that FAI contributes to the development and progression of hip arthrosis(19). Once it is accepted that FAI can eventually lead to osteoarthritis of the hip, the other major remaining question is whether "prophylactic" surgery (in asymptomatic patients) is indicated. In this regard, two reviews concluded that prophylactic surgery is not indicated, since it could be regarded as unnecessary in up to 80% of all cases(20,21). It is important to mention that despite the associations observed between FAI and coxarthrosis, most patients with radiographic FAI do not develop degenerative changes and will not require THA(19,22).
The present study has limitations, such as its retrospective design and limited number of patients. In addition, a description of the patient characteristics is lacking in the global number of surgeries. In this study we have observed a tendency towards an increased indication of hip arthroscopy in a University hospital. The literature offers no specific articles addressing changes in trend in indication or increases in the indication of hip arthroscopy versus THA. It would be interesting to conduct studies with a longer follow-up to establish the half-life of surgical success (defined as no need for further surgery), and to identify the underlying influencing factors and investigate whether they could be modified. Likewise, we wish to underscore that although there has been an increase in the indication of AHS, it cannot be affirmed that this increase has induced a decrease in the indication of THA.
Conclusion
There has been a significant increase in the use of hip arthroscopy for the treatment of FAI at our centre. Based on these results, we have observed an increase in the indication of conservative arthroscopic hip surgery and a decrease in the indication of THA at our centre, though no cause-effect relationship can be established.
Figuras
Figure 1. Flowchart showing the number of patients excluded from the final analysis of the study.
* Patients coded as presenting femoroacetabular impingement (FAI) that were operated upon for other diagnoses (diagnostic arthroscopy, intraarticular free bodies, trochanteric bursitis, snapping hip), or who underwent other procedures: diagnostic infiltrations, etc.; ** patients coded as undergoing primary total hip arthroplasty (THA) that were operated upon for other diagnoses, such as THA revision surgery, secondary coxarthrosis, proximal femoral fracture, avascular necrosis, etc.; *** FAI secondary to: epiphysiolysis, Legg-Calvé-Perthes disease, dysplasia, fracture, traumatism, osteonecrosis or infections.
Figure 2. Dot chart of the indication of total hip arthroplasty (THA) for coxarthrosis and arthroscopic hip surgery (AHS) due to femoroacetabular impingement (FAI) in patients under 60 years of age; distribution according to years.
Tablas
Información del artículo
Cita bibliográfica
Autores
Maryé Merce Méndez Ojeda
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario de Canarias. Tenerife
Universidad de La Laguna. Tenerife
Mario Herrera Pérez
Grupo de Investigación en Traumatología y Ortopedia. Universidad de La Laguna. Santa Cruz de Tenerife. Canarias
Hospital Universitario de Canarias. La Laguna. Tenerife
Tesorero de la SEMCPT
Facultad de Ciencias de la Salud. Universidad de La Laguna. Tenerife
Director de la Revista del Pie y Tobillo
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Nuestra Señora de Candelaria. La Laguna. Tenerife
Unidad Acreditada de Pie y Tobillo. HUC. Tenerife
Jorge H Núñez
Departamento de Cirugía Ortopédica. Hospital Universitario Mútua Terrassa. Barcelona
Ana M Aldea Perona
Unidad de Investigación. Parc de Salut Mar. Barcelona
Yolanda Ramallo Fariña
Fundación Canaria de Investigación Sanitaria (FUNCANIS)
Red de Investigación en Servicios de Salud en Enfermedades Crónicas (REDISSEC)
José Luis País Brito
Hospital Universitario de Canarias (HUC). Tenerife
Facultad de Ciencias de la Salud. Universidad de La Laguna. Tenerife
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323-30.
-
2Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112-20.
-
3Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264-72.
-
4Kemp JL, MacDonald D, Collins NJ, Hatton AL, Crossley KM. Hip arthroscopy in the setting of hip osteoarthritis: systematic review of outcomes and progression to hip arthroplasty. Clin Orthop Relat Res. 2015;473(3):1055-73.
-
5Frank JM, Harris JD, Erickson BJ, et al. Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A Systematic Review. Arthroscopy. 2015;31(6):1199-204.
-
6Morales-Ávalos R, Tapia-Náñez A, Simental-Mendía M, et al. Prevalence of Morphological Variations Associated With Femoroacetabular Impingement According to Age and Sex: A Study of 1878 Asymptomatic Hips in Nonprofessional Athletes. Orthop J Sport Med. 2021;9:1-14.
-
7Doherty M, Courtney P, Doherty S, et al. Nonspherical femoral head shape (pistol grip deformity), neck shaft angle, and risk of hip osteoarthritis: a case-control study. Arthritis Rheum. 2008;58(10):3172-82.
-
8Kuhns BD, Weber AE, Levy DM, Wuerz TH. The Natural History of Femoroacetabular Impingement. Front Surg. 2015;2:58.
-
9Malviya A, Raza A, Jameson S, James P, Reed MR, Partington PF. Complications and survival analyses of hip arthroscopies performed in the National Health Service in England: a review of 6,395 cases. Arthroscopy. 2015;31(5):836-42.
-
10Jamil M, Dandachli W, Noordin S, Witt J. Hip arthroscopy: Indications, outcomes and complications. Int J Surg. 2018;54(Pt B):341-4.
-
11Byrd JWT. Arthroscopic hip surgery for the treatment of femoroacetabular impingement. Orthopedics 2011;34:186-7.
-
12Khan M, Habib A, Larson CM, et al. Arthroscopy up to date: hip femoroacetabular impingement. Arthrosc J Arthrosc Relat Surg. 2016;32:177-89.
-
13Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement. Am J Sports Med 2007;35:1571-80.
-
14Bedi A, Chen N, Robertson W, Kelly BT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24(10):1135-45.
-
15Colvin AC, Harrast J, Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94(4):e23.
-
16Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29(4):661-5.
-
17Zusmanovich M, Haselman W, Serrano B, Banffy M. The Incidence of Hip Arthroscopy in Patients with Femoroacetabular Impingement Syndrome and Labral Pathology Increased by 85% Between 2011 and 2018 in the United States. Arthroscopy. 2021;S0749-8063(21)00441-2.
-
18Horner NS, Ekhtiari S, Simunovic N, Safran MR, Philippon MJ, Ayeni OR. Hip Arthroscopy in Patients Age 40 or Older: A Systematic Review. Arthroscopy. 2017;33(2):464-475.e3.
-
19Kowalczuk M, Yeung M, Simunovic N, Ayeni OR. Does Femoroacetabular Impingement Contribute to the Development of Hip Osteoarthritis? A Systematic Review. Sports Med Arthrosc Rev. 2015;23(4):174-9.
-
20Collins JA, Ward JP, Youm T. Is prophylactic surgery for femoroacetabular impingement indicated? A systematic review. Am J Sports Med. 2014;42(12):3009-15.
-
21Griffin DR, Dickenson EJ, O'Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169-76.
-
22Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91(2):162-9.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- <em>REACA</em>, the journal of everyone
- Applicability of consensus methods in hip arthroscopy: a systematic review
- Evolution of the indication of arthroscopic treatment for femoroacetabular impingement and of the indication of total hip arthroplasty in patients under 60 years of age
- Evolution of glenohumeral bone defects following failed arthroscopic Bankart repair. Study of a case series
- Important articles for the surgical treatment of lateral ankle instability
- Posterolateral elbow instability with osteochondral defect of the <em>capitellum</em>; how to deal with this combination?
- Arthroscopic treatment of a femoral osteochondroma as a cause of femoroacetabular impingement. A case report
- Arthrofibrosis in the mirror
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.