Posterolateral elbow instability with osteochondral defect of the capitellum; how to deal with this combination?
Inestabilidad posterolateral de codo con defecto osteocondral en el capitellum, ¿cómo afrontar esta asociación?
Resumen:
La lesión del complejo ligamentoso lateral tras una luxación de codo constituye una entidad de difícil manejo. Produce en el paciente episodios de luxación y subluxación repetida constituyendo una inestabilidad posterolateral rotatoria, que puede además asociar lesiones como defectos osteocondrales, secundarios a los traumatismos repetidos en la articulación durante dichas luxaciones.
Se presenta el caso de una paciente de 53 años con inestabilidad posterolateral rotatoria crónica, que además presenta un defecto osteocondral en el capitellum (lesión de Osborne-Cotterill), tras caída con el codo derecho extensión, supinación y valgo.
La paciente consulta por episodios de subluxación, semanas después de un episodio traumático, con el mecanismo de compresión axial, supinación y valgo. Se le realizó una ligamentoplastia de tipo Docking con injerto autólogo de recto interno y mosaicoplastia de 8,5 mm con injerto autólogo para cubrir el defecto del capitellum.
Las plastias para reconstruir el complejo lateral, además del uso de injertos osteocondrales para la reparación de defectos articulares extensos, se proponen aquí como una opción válida para tratar este tipo de lesiones.
Abstract:
Damage to the lateral ligament complex following elbow dislocation is difficult to manage. These lesions cause repeated luxation and subluxation episodes, producing posterolateral rotary instability that moreover may be associated to lesions such as osteochondral defects secondary to repeated trauma of the joint in the course of such luxations.
We present the case of a 53-year-old woman with chronic posterolateral rotary instability who also presented an osteochondral defect of the capitellum (Osborne-Cotterill lesion) after a fall with the right elbow in extension, supination and valgus.
The patient consulted due to subluxation episodes weeks after a traumatism involving the axial compression, supination and valgus mechanism. A Docking type ligamentoplasty was performed with autologous graft from the gracilis muscle and mosaicplasty measuring 8.5 mm with autologous grafting to cover the defect of the capitellum.
Plasty procedures to reconstruct the lateral complex, in addition to the use of osteochondral grafts to repair extensive joint defects, are proposed herein as a valid option for treating lesions of this kind.
Introduction
The elbow is the second most common joint to suffer dislocation in adults(1), representing 10-25% of all elbow injuries. Most such dislocations occur in the posterolateral or posterior direction(2).
The majority of posterior elbow luxations occur as a result of falls with the elbow in extension, through an axial compression mechanism, with the forearm in supination and valgus, giving rise to soft tissue injury that progresses in a circular manner from lateral to medial. Posterolateral rotary instability, described by O'Driscoll et al. in 1991(3), is the most common presentation following posterior elbow dislocation that has failed to respond to conservative management, and occurs due to damage to the lateral ligament complex, which is in charge of limiting external rotation of the radius and ulna with respect to the humerus, in addition to varus stress.
The by now chronic damage to the lateral collateral ligament can be resolved by means of a plasty procedure (Docking or Gong type)(4,5,6). Another option is a dynamic internal fixation system (IJS® Elbow) from Skeletal Dynamics(7,8), which is indicated for temporary use in chronic instability.
In addition, posterior elbow luxation may also involve chondral damage secondary to impingement of the radial head against the capitellum. These osteochondral defects, referred to as Osborne-Cotterill lesions, are a cause of pain and residual instability if not treated along with the rest of the elbow lesions.
We present the case of a woman with posterolateral rotary instability of the right elbow who also presented an osteochondral defect of the capitellum (Osborne-Cotterill lesion).
Clinical case
A 53-year-old woman with no relevant personal history suffered a fall with trauma of the right elbow and ankle. The patient described the fall as occurring with the shoulder raised and the elbow extended and in supination. She suffered functional impairment of the elbow, with posterior deformity of the latter. In the emergency service and following physical examination and radiographs, the patient was diagnosed with posterior dislocation of the elbow with impact fracture in the posterior region of the lateral condyle, in addition to subtalar luxation. The elbow dislocation was reduced that same day, exerting downward traction over the forearm with the elbow in 90º flexion, and with immobilisation by means of a posterior arm splint. After three weeks the patient was examined in the outpatient clinic and the splint was removed. She then started 8 weeks of rehabilitation, with a rapid gain of joint balance (0-120º).
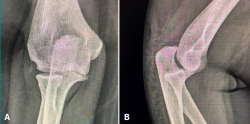
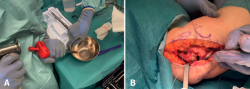
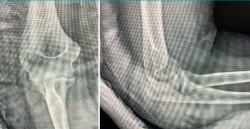
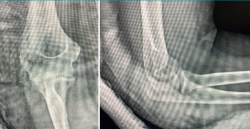
The patient was again evaluated in the clinic after 12 weeks. The physical examination revealed pain on the lateral aspect of the right elbow, with clicks on pronation, positive pivot shift manoeuvre and painful varus laxity. Complementary tests were requested: radiographs, which evidenced the Osborne-Cotterill lesion (Figure 1); a magnetic resonance imaging (MRI) scan showing distal deinsertion of the ulnar lateral collateral ligament and proximal deinsertion of the radial collateral ligament, as well as partial rupture of the annular ligament; and a computed tomography (CT) scan that found the Osborne-Cotterill osteochondral defect in the posterior capitellum to measure 8 × 3 mm (Figure 2). The patient suffered another posterior dislocation episode the following week after a new fall while undergoing rehabilitation. A second closed reduction was therefore performed.
In total, she experienced three further subluxation episodes in these weeks. In view of the great instability, surgical treatment was decided 6 months after the initial injury. The operation consisted of Docking type ligamentoplasty with an autologous graft from the gracilis muscle of the right knee and mosaicplasty measuring 8.5 mm in diameter with autologous grafting from the same knee.
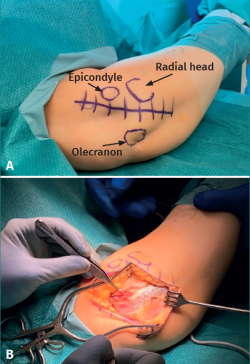
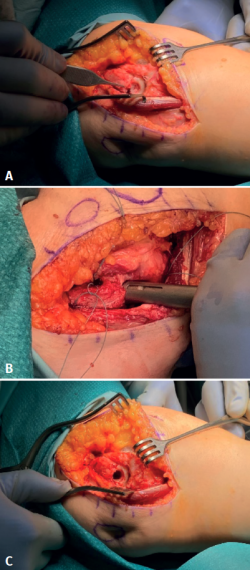
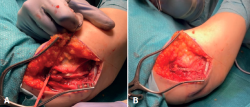
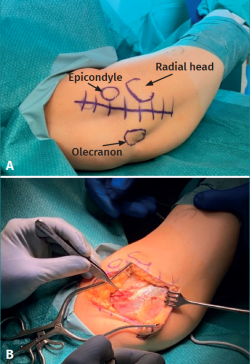
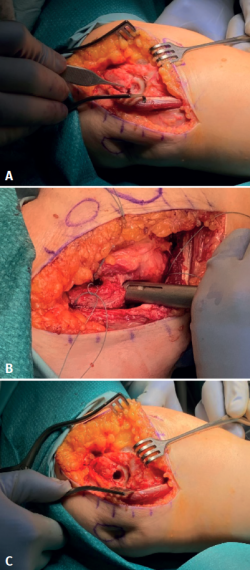
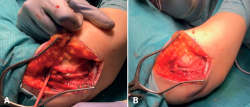
With the patient in supine decubitus, and following general anaesthesia with ischemia of the root of the right arm, a 5-cm longitudinal incision was made over the lateral column of the humerus (Figure 3A) with a Kocher approach between the anconeus and extensor carpi ulnaris (Figure 3B), raising the anconeus from the ulna until exposing the posterior part of the joint. The bone bed in the receptor zone (capitellum) measured 8 mm in diameter and 3 mm in depth (Figure 4A). This bed was prepared for the mosaicplasty (Figures 4B and 4C).
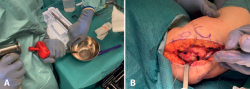
The osteochondral graft was then harvested. It was obtained from the lateral femoral trochlea, as this is not a weight-bearing zone, and thus constitutes a good bone and cartilage donor site. The Mosaicplasty® system of Smith & Nephew was used for this purpose, through an open arthrotomy measuring about 2 cm, yielding an 8.5-mm cylinder (Figure 5A) that was impacted in the prepared receptor zone (Figure 5B).
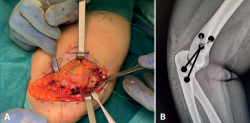
The ulnar tunnels for passing the tendon graft were required to be convergent and measured 3.5 mm in diameter, and were made following the introduction of Kirschner pins with the use of cannulated drills (Figures 6A and 6B): the more distal at the level of the supinator crest and the proximal at the level of the insertion of the annular ligament, taking care to leave a 1.5-cm bone bridge between them. The humeral tunnels presented a "Y" configuration. The more distal tunnel measured 4.5 mm and was made at the isometric point, while the other two (one anterior and the other posterior) measured 3.5 mm in diameter and were located more proximal and convergent to the first tunnel.
reacae.29377.fs2206008en-figure6.png
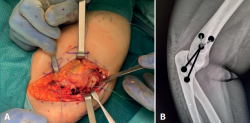
Figure 6. The ulnar tunnels were prepared as follows: the more distal at the level of the supinator crest and the more proximal at the level of the insertion of the annular ligament, leaving a 1.5-cm bone bridge between them, so that they are convergent. Humeral tunnels: one measuring 4.5 cm made at the isometric point, and another two proximal and convergent to the first tunnel, measuring 3.5 cm in "Y" configuration.
The plasty was prepared with Krackow sutures at the extremities, and suture loops were left in the tunnels to serve as transporters.
Once the plasty was passed through the ulnar tunnels, its extremities were crossed and both were inserted through the distal humeral tunnel, with each extremity emerging from one of the proximal orifices (Figure 7).
At this point the extremities were joined using Ethibond suture with the elbow flexed 40º and in pronation, leaving the plasty in an extraarticular position (Figures 8A and 8B).
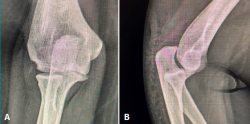
Following an immediate postoperative period (Figure 9) without complications and with adequate rehabilitation, the patient has been able to return to her normal life four and a half months after surgery. Upon exploration, the elbow proved stable, with a full joint motion range, and the patient was able to perform axial loading without pain or failure sensation (Figures 10A and 10B). The radiographs evidenced the reduced elbow (Figure 11).
Discussion
Chronic posterior dislocation of the elbow requiring surgical treatment, as in our case, is an infrequent condition. This combined lesion (osteochondral defect of the capitellum and damage to the lateral collateral ligament [LCL]) was resolved by mosaicplasty and Docking ligamentoplasty, with a good postoperative outcome. Good understanding of the characteristics of the lesion (i.e., direction of the luxation, soft tissue lesion features and stability after reduction) is important for deciding the most effective treatment in such cases.
The ligaments enveloping the lateral capsule of the elbow are the LCL or radial ligament, the ulnar LCL (ULCL), the accessory LCL and the annular ligament. In addition to stabilising the lateral aspect of the elbow, the ULCL acts as a posterior stop for the radial head, avoiding its subluxation(9). On flexing the elbow, damage to the ULCL causes the ulna to undergo anomalous supination over the humerus, with posterior and lateral subluxation of the radial head, associated to both ulnar and radial displacement in external rotation and valgus.
In isolated luxation of the radial head, the proximal radioulnar joint ruptures, while the humeroulnar joint remains intact. In contrast, in posterolateral rotary instability, the proximal radioulnar joint is preserved and the two bones of the forearm rotate as a single unit(10).
According to Horii(11), the pathophysiology of elbow instability can be explained by considering that the joint is a circle that ruptures in three stages. Stage 1 is characterised by ULCL rupture, producing posterolateral subluxation of the radial head upon supination of the elbow. If the lesion progresses medially, the anterior capsule and posterior capsule of the elbow rupture; the humeroulnar joint experiences subluxation, and the coronoid process becomes trapped in the humeral trochlea (stage 2). If the force progresses, the elbow suffers complete dislocation(12). This last stage in turn is divided into substage 3a, characterised by soft tissue involvement, except for the anterior band of the medial collateral ligament. In substage 3b the anterior band also ruptures, leaving the elbow unstable in valgus. Lastly, in substage 3c, the elbow is completely unstable multi-directionally. This model of the circle of Horii is analogous to the perilunar instability pattern of Mayfield seen in the wrist(13).
Posterolateral rotary instability occurs as a result of damage to the lateral ligament complex of the elbow following trauma-induced dislocation combining axial compression + supination + valgus over the elbow(14). Such posterolateral instability occurs in less than 10% of all cases of elbow dislocation(12). Following a first elbow dislocation episode, conservative management(15) with two weeks of sling immobilisation followed by early rehabilitation usually proves effective(16,17). However, early subluxation or recurrent luxation, as in our case, indicates a lack of healing of the lateral ligament complex, and the manifestation of mechanical pain and varus laxity (on reaching half of the range of extension with the forearm in supination) suggests posterolateral rotary instability, pointing to the advisability of surgical treatment(14).
Reconstruction of the ligament should be anatomical, isometric and extracapsular(12). The most common practice is to recreate the ULCL via a ligamentoplasty with an autologous or heterologous tendon graft that is usually tunnelled and sutured onto itself - location of the isometric point in the humerus being a critical point of surgery. This is done with the elbow flexed and in full pronation(10). It is not always necessary to repair the medial collateral complex, because the elbow may be stable after repairing the LCL complex and extensor musculature, as in our case. The Kocher or posterolateral approach was used in surgery. Consideration is required of possible damage to the posterior interosseous nerve, which can be avoided through pronation of the forearm(2).
Damage to the capitellum secondary to elbow dislocation may go unnoticed on plain X-rays. In this respect, MRI or CT, with a strong clinical suspicion, are needed to establish the diagnosis. Hyojune Kim et al. (2020) found osteochondral lesions in 48.8% of their cases, using MRI, in patients that had suffered simple elbow luxation. Most of these lesions were observed in the posterolateral region of the capitellum(18). However, it is not common to identify an osteochondral defect as large as that seen in our patient, which measured 8 × 3 mm in the posterior region of the capitellum.
Mosaicplasty with autologous osteochondral grafting has been well described in defects of the knee, hip and ankle(19,20), though it has been little mentioned in the elbow(21,22). In contrast, the reconstruction of defects of the coronoid process using radial head autologous grafts has been widely described at elbow level(23,24,25). The capitellum defects described in the literature refer fundamentally to osteochondritis dissecans in young patients and athletes(26). Yamaga et al. (2018) reported good clinical outcomes after covering osteochondral defects of the capitellum in two patients using autologous grafts from the knee(27). Resolution with femoral trochlea grafts is a valid alternative which we considered in this case as a viable treatment option.
Conclusion
Posterolateral rotary instability after conservative management of posterior dislocation is not a common condition in clinical practice. Plasty surgery to reconstruct the lateral complex, in addition to the use of osteochondral grafts to repair joint defects, is a valid option that proves technically demanding from the surgical perspective but affords good long-term outcomes for the patient.
Figuras
Figure 1. A: anteroposterior X-ray showing the Osborne-Cotterill lesion; B: lateral X-ray view of the elbow subluxation with the impacted radial head.
Figure 2. Coronal and sagittal computed tomography views showing a bone defect in the capitellum measuring 10 × 8 × 3 mm.
Figure 3. First incision and Kocher approach. A: 5-cm longitudinal skin incision on lateral surface of elbow. The anatomical references of the radial head, epicondyle and olecranon are marked; B: Kocher approach between the anconeus and extensor carpi ulnaris.
Figure 4. A: bone bed of the receptor zone (Osborne-Cotterill lesion in the capitellum) measuring 8 × 3 mm in depth; B and C: preparation of the bed for mosaicplasty with an external femoral trochlea graft.
Figure 5. The graft is harvested from the femoral trochlea (A), obtaining a cylinder that is impacted in the prepared receptor zone (B).
Figure 6. The ulnar tunnels were prepared as follows: the more distal at the level of the supinator crest and the more proximal at the level of the insertion of the annular ligament, leaving a 1.5-cm bone bridge between them, so that they are convergent. Humeral tunnels: one measuring 4.5 cm made at the isometric point, and another two proximal and convergent to the first tunnel, measuring 3.5 cm in "Y" configuration.
Figure 7. Once the ligament was passed through the ulnar tunnels, the extremities were crossed and both were inserted through the tunnel at the isometric point, with each extremity emerging from one of the proximal orifices.
Figure 8. The extremities were joined using Ethibond suture with the elbow flexed 40º and in pronation.
Figure 10. Final postoperative view of the patient four and a half months after surgery, with full motion range.
Información del artículo
Cita bibliográfica
Autores
María Mercedes Batista Hernández
Hospital Maz. Zaragoza
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario de Badajoz
Santos Moros Marco
Servicio de Traumatología. Hospital MAZ. Zaragoza
Cirugía Ortopédica y Traumatología. Unidad de Miembro Superior. Hospital MAZ Zaragoza. Arthrosport Zaragoza
Editor asociado de REACA
Servicio de Traumatología y Cirugía Ortopédica. Hospital de la Mutua MAZ. Zaragoza
José Luis Ávila Lafuente
Unidad de Cirugía de Hombro y Codo. Servicio de Traumatología. Hospital MAZ. Zaragoza
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Maripuri SN, Debnath UK, Rao P, Mohanty K. Simple elbow dislocation among adults: a comparative study of two different methods of treatment. Injury. 2007 Nov;38(11):1254-8.
-
2Fenelon C, Zafar MM, Sheridan GA, Kearns S. Irreducible posterolateral elbow dislocation: a rare injury. BMJ Case Rep. 2016 Dec 30;2016:bcr2016217967.
-
3O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotator instability of the elbow. J Bone Joint Surg Am. 1991;73:440-6.
-
4Gong HS, Kim JK, Oh JH, Lee YH, Chung MS, Baek GH. A New Technique for Lateral Ulnar Collateral Ligament Reconstruction Using the Triceps Tendon. Tech Hand Up Extrem Surg. 2009 Mar;13(1):34-6.
-
5Sánchez-Sotelo J, Morrey BF, O’Driscoll SW. Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow. J Bone Joint Surg Br. 2005;87:54-61.
-
6O’Driscoll SW. Reconstruction of the lateral collateral ligament. En: Yamaguchi K, King GJ, McKee M, et al. (eds.). Advanced Reconstruction. Elbow. Rosemont, IL: AAOS; 2007. pp. 159-65.
-
7Orbay JL, Ring D, Kachooei AR, et al. Multicenter trial of an internal joint stabilizer for the elbow. J Shoulder Elbow Surg. 2017 Jan;26(1):125-32.
-
8Sochol KM, Andelman SM, Koehler SM, Hausman MR. Treatment of Traumatic Elbow Instability With an Internal Joint Stabilizer. J Hand Surg Am. 2019 Feb;44(2):161.
-
9Mehta JA, Bain GI. Posterolateral Rotatory Instability of the Elbow. J Am Acad Orthop Surg. 2004;12:405-15.
-
10Charalambous CP, Stanley JK. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Br. 2008;90-B:272-9.
-
11O’Driscoll SW, Morrey BF, Korinek S, Ann KN. Elbow subluxation and dislocation: a spectrum of instability. Clin Orthop. 1992;280:167-97.
-
12Gallucci GL, Rellán I, Boretto JG, Alfie VA, Donndorff A, De Carli P. Inestabilidad posterolateral crónica de codo. Reconstrucción ligamentosa. Rev Asoc Argent Ortop Traumatol. 2016;4:294-301.
-
13Mehta JA, Bain GI. Posterolateral Rotatory Instability of the Elbow. J Am Acad Orthop Surg. 2004;12:405-15.
-
14Moros Marco S, Asenjo Gismero CV, del Monte Bello G, et al. Epicondilitis (tendinopatía lateral de codo): estrategias de diagnóstico y clasificación. Rev Esp Artrosc Cir Articul. 2020;27(4):317-38.
-
15Cho CH, Kim BS, Rhyou IH, et al. Posteromedial Elbow Dislocations without Relevant Osseous Lesions Clinical Characteristics, Soft-Tissue Injury Patterns, Treatments, and Outcomes. J Bone Joint Surg Am. 2018;100:2066-72.
-
16Maripuri SN, Debnath UK, Rao P, Mohanty K. Simple elbow dislocation among adults: a comparative study of two different methods of treatment. Injury. 2007;38:1254-8.
-
17Schubert I, Strohm PC, Maier D, Zwingmann J. Simple traumatic elbow dislocations; benefit from early functional rehabilitation. Medicine (Baltimore). 2021 Nov 5;100(44):e27168.
-
18Kim H. Distribution of Osteochondral Lesions in Patients With Simple Elbow Dislocations Based on MRI Analysis. Orthop J Sports Med. 2020;8(8):2325967120946269.
-
19Hangody L, Ráthonyi GK, Duska Z, Vásárhelyi G, Füles P, Módis L. Autologous osteochondral mosaicplasty. Surgical technique. J Bone Joint Surg Am. 2004 Mar;86-A Suppl 1:65-72.
-
20Kodama N, Honjo M, Maki J, Hukuda S. Osteochondritis dissecans of the talus treated with the mosaicplasty technique: a case report. J Foot Ankle Surg. 2004:43:195-8.
-
21Iwasaki N, Kato H, Ishikawa L, Masuko T, Funakoshi T, Minami A. Autologous Osteochondral Mosaicplasty for Osteochondritis Dissecans of the Elbow in Teenage Athletes. J Bone Joint Surg. 2009;91A(10).
-
22Nikolaoua VS, Giannoudis PV. History of osteochondral allograft transplantation. Injury. 2017;48(7):1283-6.
-
23Ring D, Guss D, Jupiter JB. Reconstruction of the coronoid process using a fragment of discarded radial head. J Hand Surg Am. 2012;37:570-4.
-
24Van Riet RP, Morrey BF, O’Driscoll SW. Use of osteochondral bone graft in coronoid fractures. J Shoulder Elbow Surg. 2005;14:519-23.
-
25Bellato E, Rotini R, Marinelli A, Guerra E, O’Driscoll SW. Coronoid reconstruction with an osteochondral radial head graft. J Shoulder Elbow Surg. 2016 Dec;25(12):2071-7.
-
26Baker CL 3rd, Baker CL Jr, Romeo AA. Osteochondritis dissecans of the capitellum. J Shoulder Elbow Surg. 2010;19:76-82.
-
27Yamaga T, Horii E, Koh S, Sugiura H. Osteochondritis dissecans of the capitellum secondary to fishtail deformity treated with osteochondral autograft. JSES Open Access. 2018 Apr 10;2(2):126-8.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- <em>REACA</em>, the journal of everyone
- Applicability of consensus methods in hip arthroscopy: a systematic review
- Evolution of the indication of arthroscopic treatment for femoroacetabular impingement and of the indication of total hip arthroplasty in patients under 60 years of age
- Evolution of glenohumeral bone defects following failed arthroscopic Bankart repair. Study of a case series
- Important articles for the surgical treatment of lateral ankle instability
- Posterolateral elbow instability with osteochondral defect of the <em>capitellum</em>; how to deal with this combination?
- Arthroscopic treatment of a femoral osteochondroma as a cause of femoroacetabular impingement. A case report
- Arthrofibrosis in the mirror
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.