Alteration of the coronal and sagittal axes of the knee and its implication in the failure of anterior cruciate ligament reconstruction. A systematic review
Alteración de los ejes coronal y sagital de la rodilla y su implicación en el fracaso de la reconstrucción de cruzado anterior. Revisión sistemática
Resumen:
Objetivo: analizar la evidencia científica disponible en cuanto a la implicación de las alteraciones en los ejes coronal y sagital de la rodilla como causa de fracaso tras la reconstrucción del ligamento cruzado anterior (LCA) y el impacto de la adición de osteotomías correctoras sobre los resultados clínicos y funcionales de la reconstrucción del LCA en presencia de dichas desalineaciones, tanto en cirugía primaria como de revisión.
Métodos: se realizó una revisión sistemática de la literatura sobre la relación entre las alteraciones en la alineación de la rodilla y el fracaso de la cirugía reconstructiva del LCA. Para ello, conforme a las guías PRISMA (Preferred Reporting Items for Systematic Reviews), se han realizado búsquedas en las bases de datos Medline, PubMed y Embase, incluyendo estudios centrados en osteotomías de rodilla realizadas de forma conjunta o secuencial a cirugía de revisión del LCA, en pacientes esqueléticamente maduros.
Resultados: se incluyeron 14 estudios que analizaron el perfil sagital y 8 que analizaron el coronal. En los que analizaron el perfil sagital, 11 de ellos recomiendan la osteotomía de deflexión de la rodilla como tratamiento para cirugía de rescate tras fracaso de ligamentoplastia de cruzado anterior de la rodilla cuando existen aumentos de la pendiente tibial mayores de 12°. En cuanto a los estudios que analizaron el perfil coronal, todas las publicaciones, salvo una, encontraron diferencias en los resultados tras añadir una osteotomía tibial en cirugía de revisión del LCA de rodillas varas. Estos estudios concluyeron que la corrección del varo mejora la funcionalidad y la estabilidad de esas rodillas. Los resultados de la cirugía combinada, tanto objetivos como subjetivos y de retorno a la actividad deportiva, fueron buenos.
Conclusiones: la osteotomía tibial proximal es un tratamiento efectivo en el tratamiento de rodillas con inestabilidad anterior asociadas a alteraciones del plano coronal y sagital.
Nivel de evidencia: 4.
Relevancia clínica: en la cirugía de revisión del LCA es importante analizar las desviaciones de la alineación de la rodilla. Si corregimos estas desviaciones en la cirugía de revisión del LCA, obtendremos mejores resultados.
Abstract:
Objective: to analyse the available scientific evidence regarding the implication of alterations of the coronal and sagittal axes of the knee as a cause of failure after anterior cruciate ligament (ACL) reconstruction and the impact of the addition of corrective osteotomies on the clinical and functional outcomes of ACL reconstruction in the presence of such misalignments, in both primary and revision surgery.
Methods: A systematic review was made of the literature on the relationship between alterations in knee alignment and the failure of ACL reconstructive surgery. In accordance with the PRISMA(Preferred Reporting Items for Systematic Reviews) statement, the Medline, PubMed and Embase databases were searched, including studies focusing on knee osteotomies performed in conjunction or sequentially to ACL revision surgery in skeletally mature patients.
Results: A total of 14 studies analysing the sagittal profile and 8 analysing the coronal profile were included. Of the studies that analysed the sagittal profile, 11 recommended knee deflexion osteotomy in salvage surgery after failed anterior cruciate ligamentoplasty of the knee in the presence of tibial slope increments of over 12°. Regarding the studies that analysed the coronal profile, all but one publication found differences in outcomes after the addition of a tibial osteotomy in ACL revision surgery of varus knees. These studies concluded that varus correction improves the functionality and stability of these knees. The outcomes of combined surgery, both objective and subjective, and referred to the return to sports activity, were good.
Conclusions: Proximal tibial osteotomy is an effective treatment in the management of knees with anterior instability associated with alterations of the coronal and sagittal planes.
Level of evidence: Level 4.
Clinical relevance: In ACL revision surgery it is important to analyse deviations in knee alignment. Correcting these deviations in ACL revision surgery will lead to better outcomes.
Introduction
Anterior cruciate ligament (ACL) reconstruction is a widely accepted procedure for the treatment of ACL tears, although it has a 10-20% failure rate at 10 years(1). The results of these revision surgeries are worse than those of primary surgery, with only 27% of patients returning to their previous level of activity(2) and re-rupture rates of up to 12%(1).
There are multiple causes related to the failure of ACL reconstruction, including a new traumatic event, errors in surgical technique, infections, biological failures... and, in up to 4% of cases, alterations in the alignment of the knee(1).
Until a few years ago, osteotomies have been used for the treatment of monocompartmental osteoarthritis associated with varus or valgus alignment of the knee because of their role in load distribution, "relieving" the load on the affected compartment in cases of degenerative disease(3).
Recently, tibial slope has been linked to centre pivot mechanics. Several biomechanical studies on cadaveric specimens have studied the association between sagittal plane deaxations and failure of ACL plasty: Agneskirchner et al.(4) demonstrated in 2004 the relationship between posterior tibial slope values and the tensile forces experienced by both cruciate ligaments, and, in the same year, Giffin et al.(5) showed how decreasing or increasing this slope can improve knee biomechanics and decrease stress on the ACL or posterior cruciate ligament (PCL).
Alignment in the coronal plane also plays a determinant role in the biomechanics of the cruciate ligaments: chronic ACL tears lead to deterioration of the cartilage in the posterior region of the internal tibial plateau, resulting in progressive varus deviation (simple or primary varus) which, over time, will lead to weakening of the lateral ligamentous structures (double varus), characterised by the appearance of a "dynamic varus thrust" under load. In the final stage, the failure of the stabilisers of the posteroexternal corner will result in a triple varus deformity, manifested by a "varus-recurvatum thrust" phenomenon during gait. Several biomechanical studies have shown an increase in the stresses suffered by the ACL(6) in double and triple strains, favouring its rupture (and that of its reconstructions). Won(7) and Noyes(8) demonstrated an increased frequency of varus misalignments in patients requiring ACL revision surgery and Kim et al.(9) demonstrated that inadvertent tibial slope augmentation during proximal tibial valgus osteotomies causes degenerative changes in the ACL.
This is why the paradigm of the role of proximal tibial osteotomy has changed, expanding its range of indications beyond single-compartment osteoarthritis. The 3 objectives of osteotomy in unstable knees are: to prevent progression of osteoarthritis due to joint wear and tear(10), to protect the plasty from overloading the misaligned knee and to restore stability(11).
The aim of this study is to perform a systematic review of the literature on the results of this surgery in patients with previous ACL reconstruction surgery who present instability after surgical stabilisation. For this purpose, we analysed the postoperative results of limb realignment surgery in these indications, referring to stability (objective and subjective), degree of satisfaction, return to daily activities and sports, as well as associated complications.
Methods
This systematic review was conducted in accordance with PRISMA(Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Bibliographic search
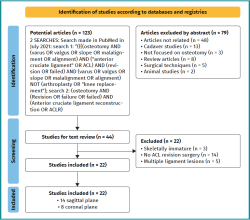
We conducted a systematic electronic database search in Medline, PubMed and Embase in July 2021 to identify clinical studies related to: 1) knee axis alterations as a cause of failure after ACL reconstruction surgery; and 2) the impact of surgical realignment procedures on knee instability after ACL stabilisation surgery. Searches were carried out using the following headings and fields. Search 1: (osteotomy) AND (varus OR valgus OR slope OR malalignment OR alignment) AND ("anterior cruciate ligament" OR ACL) AND (revision OR failed) AND (varus OR valgus OR slope OR malalignment OR alignment) NOT (arthroplasty OR "knee replacement"); search 2: (osteotomy) AND (revision OR failure OR failed) AND (anterior cruciate ligament reconstruction OR ACLR).
Inclusion criteria consisted of: studies focusing on sagittal and coronal plane alterations as a cause of failure after ACL reconstruction surgery and studies including outcomes of ACL reconstruction surgery in conjunction with corrective tibial osteotomies, both with a minimum follow-up of 2 years, skeletally mature patients, English language and human studies. Exclusion criteria included animal studies, basic science studies, cadaveric studies, editorials, reviews, expert opinions, surveys, topical issues and letters to the editor. We also excluded all studies that did not focus on the knee joint. In addition, all references of included studies were reviewed.
Data extraction
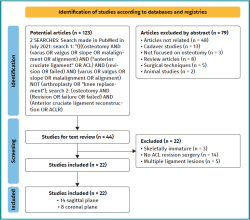
We performed data extraction according to the inclusion and exclusion criteria, as reflected in the PRISMA flow chart (Figure 1). All studies were assessed by two independent investigators (JDR and PC). The summaries of the rest of the studies were read. If there was doubt as to whether the study met the inclusion criteria, the full study was read. The level of evidence of all articles was studied according to Wright's definition(12) published in the Journal of Bone & Joint Surgery. We collected the information obtained from the studies. We assessed pre- and postoperative instability, subjective as well as objective instability sensation with anterior drawer test, Lachman and pivot shift. We measure both coronal and sagittal misalignment, as well as satisfaction and complications. These data were recorded in a Microsoft Excel spreadsheet (Microsoft Corp.).
Bias
In level 3 and 4 studies, it is logical to think that selection biases may exist, due to the lack of randomisation and prospective control groups, especially in populations with heterogeneity of their lesions. We limit this point by ensuring that the authors minimised this bias while admitting the limitations of their study in the publications.
RESULTS
Through manual and electronic reference searching, a total of 123 potentially valid studies were identified. Following the detailed review in Figure 1, we finally included 22 articles, of which 14 dealt with the sagittal profile and 8 with the coronal profile. This gave us a number of 3,925 patients in the sagittal profile group and 563 patients in the coronal profile group. Follow-up of patients ranges from 2 to 23 years. There was heterogeneity in terms of indications, objective and subjective outcomes within the included studies. The most commonly used measurements during patient follow-up were subjective (patient-perceived) and objective (by anterior drawer, Lachman and pivot shift measurement) instability, return to sport and complications. The choice of satisfaction parameters was also varied.
Sagittal profile
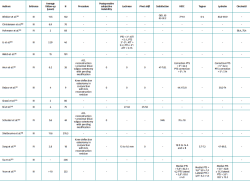
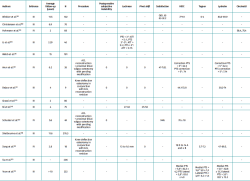
We found 14 articles that met the inclusion criteria. In 11 of them, they recommend knee deflection osteotomy as a treatment for salvage surgery after failed anterior cruciate ligamentoplasty of the knee when there are tibial slope increases. Of these, 3 found no differences in the groups studied. Regarding the limiting value for correction, it seems to be quite widespread that for slopes steeper than 12° , correction may be justified to increase the survival of the plasty. In one study, by Yoon et al.(13), they used Li's criteria arbitrarily as reference values. Regarding the technique of choice for tibial slope measurement, there is considerable heterogeneity in the articles. For most authors, Hudek's method(14), based on magnetic resonance imaging (MRI), is the most accurate, although only 5 of these studies used this form of measurement. Lateral full tibia radiographs were used in 2 studies and lateral short tibia radiographs in 7 studies. As for the results, 8 of the studies do not define the method of measuring the degree of subjective satisfaction, 6 of them use scales such as the International Knee Documentation Committee (IKDC) or the Lysholm scale, and 7 of them do not describe satisfaction measurement scales (Table 1)(13,15-27).
Coronal profile
There are 8 articles included in the review (Table 2)(25,28,29,30,31,32,33,34). All but one publication found differences in outcomes after the addition of a tibial osteotomy in revision ACL surgery of varus knees. These studies concluded that varus correction improves the functionality and stability of these knees. As for the measurement technique, in 6 of them it was the mechanical femorotibial angle measured in anteroposterior radiography of the lower limbs under load. One of them used the mechanical axis deviation and one did not define it. None of the articles describe the correction cut-off point.
Satisfaction
All studies used scales such as the IKDC, Lysholm and/or Tegner scales, although in 3 of them objective instability measures were not defined. As limitations, they show series with little follow-up, retrospective and, in half of them, without a control group.
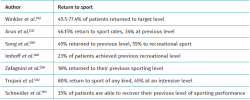
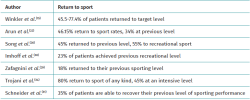
Return to sport
They vary between 18 and 80%, although the definition criteria are heterogeneous and sometimes arbitrary, making comparability very limited (Table 3)(15,22,26,28,29,31,34).
Complications
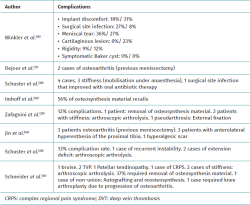
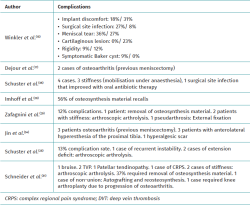
Most of the reviewed studies on coronal profile alterations include a description of the complications, although only 3 of those analysing sagittal profile alterations did so. One study shows a 10% complication rate(15), including stiffness and superficial infections. In another(29), discomfort from osteosynthesis material and superficial infection were the most frequent. In the remaining studies, complications were either not assessed or not specifically described in their text.
Of those who assessed the coronal profile, 5 of them reflect complications. One study(30) shows up to 12% complications (discomfort from osteosynthesis material, stiffness or pseudarthrosis) and another(35) 13% complications, ranging from instability to stiffness. One case of surgical wound hyperesthesia, one case of postoperative pain and one case of persistent varus due to hypocorrection are described. Of note is the article by Schneider(31), where 37% complained of discomfort from the implant and one patient required revision surgery with total knee arthroplasty (Table 4)(15,17,25,28,29,31,34,35).
Discussion
The most important finding of this study is that after ACL plasty rupture and in the presence of a coronal or sagittal axis disturbance, ACL revision surgery together with knee osteotomy improves patients' objective and subjective scales.
The study of axis alterations should be systematically included in the preoperative imaging protocol. In the event that this alteration is confirmed and in line with the findings obtained from this systematic review, limb realignment surgery should be considered and performed either in isolation or in combination with ACL revision surgery(14).
This can be performed alone, as an associated gesture or in 2 stages, preceded by ACL salvage surgery in cases of persistent instability. On this last point, there are contradictory results. In the Shelbourne study(16), despite acknowledging that increased slope is associated with an increased risk of ACL plasty rupture, they do not recommend prophylactic corrective osteotomy or primary surgery, as the risk of rupture of the contralateral ACL or revision plasty is low. In addition, the complication rate is not negligible, with a 13% complication rate (although generally minor); and up to 56% of patients will receive a second surgery for removal of the osteosynthesis material, due to discomfort with it.
In Winkler's study(15), it can be seen how patients with tibial slope above12° have higher failures and worse results in objective and subjective tests, recommending realignment surgery to improve these assessment parameters. Dejour et al.(17) evaluated the results of ACL revision surgery in conjunction with knee deflection osteotomy, with a minimum follow-up of 2 years, concluding that this tibial slope correction surgery protects the plasty from biomechanical overloads. Giffin et al.(5), in a biomechanical study, demonstrate that an increase in this slope leads to an anterior tibial translation at rest, which increases with load. Their findings suggest that decreasing this slope may have a protective effect in the ACL-deficient knee. Furthermore, just as decreasing the tibial slope has a protective effect on the ACL, the same effect on the PCL can be expected if the posterior tibial slope is increased. This may be an alternative for older patients with degenerative changes in whom ACL reconstructive surgery is a relative contraindication.
With regard to the coronal plane, Zaffagnini et al.(17) combine ACL revision surgery with proximal tibial valgus osteotomy, obtaining improvements in functional, stability and alignment results, although they concluded that once monocompartmental osteoarthritis was established, the realignment osteotomy did not prevent the progression of these degenerative changes in the medial compartment. Even so, they improve all parameters and achieve a return to sport of 20%.
It is evident that, despite complications, realignment surgery in conjunction with ACL revision improves functional outcomes and has good rates of return to sport, reaching rates of 18-80%(15,22,26,28,29,31,34), as can be seen in this systematic review. Studies evaluating the combination of ACL revision surgery and anterior tibial osteotomy tended to report higher postoperative activity levels compared to osteotomy alone. However, postoperative activity scores on the Tegner scale improved in all groups of patients, even those with ACL insufficiency who were treated by osteotomy alone. This highlights the importance of correct alignment for the performance of activities of daily living, as misalignments can lead to pain both from overloading one of the compartments and from ligamentous stress and the associated feeling of instability, which adds to the incompetence of the ACL. This review concludes that there is an increased likelihood of failure of ACL reconstruction surgery in the presence of misalignments in the coronal and/or sagittal planes of the knee. Furthermore, current literature suggests that, in these cases, the addition of a corrective tibial osteotomy may reduce this risk. However, there is currently a lack of comparative studies between isolated ACL reconstruction surgery and combined surgery with tibial osteotomy, which are essential for a complete assessment of the risk-benefit profile of both options.
There are several limitations to this study. First, this systematic review almost exclusively includes studies with levels 3 and 4 evidence (prospective and retrospective series). Second, many of the studies evaluated are more than 10 years old. In addition, data collection and outcome assessment parameters were quite heterogeneous, making it difficult to infer results. Third, a large number of the studies had selection biases due to their non-randomised design and lack of a prospective control group.
Conclusions
Proximal tibial osteotomy is an effective treatment in the management of knees with anterior instability associated with coronal and sagittal plane disturbances.
Información del artículo
Cita bibliográfica
Autores
Jaime Dalla Rosa Nogales
Hospital Quirónsalud Málaga
Hospital Vithas Parque San Antonio. Málaga
Complejo Hospitalario Integral Privado (CHIP). Málaga
Agencia Sanitaria Costa del Sol. Marbella, Málaga
Pablo Crespo Hernández
Sección de Miembro Inferior. Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Ramón y Cajal, Madrid
Editor invitado
Hospital Universitario HM-Sanchinarro. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(9):1566-71.
-
2Griffith TB, Allen BJ, Levy BA, Stuart MJ, Dahm DL. Outcomes of repeat revision anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:1296-301.
-
3Feller JA, Webster KE, Slullitel D, Galan H. Controversies in the Technical Aspects of ACL Reconstruction. Springer Berlin Heidelberg. 2017;44:477-89.
-
4Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124:575-84.
-
5Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376-82.
-
6Van de Pol GJ, Arnold MP, Verdonschot N, van Kampen A. Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med. 2009;37:481-7.
-
7Won HH, Chang CB, Je MS, Chang MJ, Kim TK. Coronal limb alignment and indications for high tibial osteotomy in patients undergoing revision ACL reconstruction. Clin Orthop Relat Res. 2013;471:3504-11.
-
8Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000;28:282-96.
-
9Kim GB, Kim KI, Song SJ, Lee SH. Increased Posterior Tibial Slope After Medial Open-Wedge High Tibial Osteotomy May Result in Degenerative Changes in Anterior Cruciate Ligament. J Arthroplasty. 2019;34(9):1922-8.
-
10Kim SJ, Moon HK, Chun YM, Chang WH, Kim SG. Is correctional osteotomy crucial in primary varus knees undergoing anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2011;469:1421-6.
-
11Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32:60-70.
-
12Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85-A:1-3.
-
13Yoon KH, Park SY, Park JY, et al. Influence of Posterior Tibial Slope on Clinical Outcomes and Survivorship After Anterior Cruciate Ligament Reconstruction Using Hamstring Autografts: A Minimum of 10-Year Follow-Up. Arthroscopy. 2020;36(10):2718-27.
-
14Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066-72.
-
15Winkler PW, Wagala NN, Hughes JD, Lesniak BP, Musahl V. A high tibial slope, allograft use, and poor patient-reported outcome scores are associated with multiple ACL graft failures. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):139-48.
-
16Shelbourne KD, Benner RW, Jones JA, Gray T. Posterior Tibial Slope in Patients Undergoing Anterior Cruciate Ligament Reconstruction With Patellar Tendon Autograft: Analysis of Subsequent ACL Graft Tear or Contralateral ACL Tear. Am J Sports Med. 2021;49(3):620-5.
-
17Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23:2846-52.
-
18Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:2510-4.
-
19Hohmann E, Bryant A, Reaburn P, Tetsworth K. Does posterior tibial slope influence knee functionality in the anterior cruciate ligament deficient and anterior cruciate ligament-reconstructed knee? Arthroscopy. 2010;26:1496-502.
-
20Li Y, Hong L, Feng H, et al. Posterior tibial slope influences static anterior tibial translation in anterior cruciate ligament reconstruction: a minimum 2-year follow-up study. Am J Sports Med. 2014;42:927-33.
-
21Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament–reconstructed patient. Am J Sports Med. 2013;41:2800-4.
-
22Arun GR, Kumaraswamy V, Rajan D, et al. Long-term follow up of single-stage anterior cruciate ligament reconstruction and high tibial osteotomy and its relation with posterior tibial slope. Arch Orthop Trauma Surg. 2016;136:505-11.
-
23Grassi A, Signorelli C, Urrizola F, et al. Patients With Failed Anterior Cruciate Ligament Reconstruction Have an Increased Posterior Lateral Tibial Plateau Slope: A Case-Controlled Study. Arthroscopy. 2019;35(4):1172-82.
-
24Ni QK, Song GY, Zhang ZJ, et al. Steep Posterior Tibial Slope and Excessive Anterior Tibial Translation Are Predictive Risk Factors of Primary Anterior Cruciate Ligament Reconstruction Failure: A Case-Control Study With Prospectively Collected Data. Am J Sports Med. 2020;48(12):2954-61.
-
25Schuster P, Geßlein M, Schlumberger M, Mayer P, Richter J. The influence of tibial slope on the graft in combined high tibial osteotomy and anterior cruciate ligament reconstruction. Knee. 2018;25(4):682-91.
-
26Song GY, Ni QK, Zheng T, Zhang ZJ, Feng H, Zhang H. Slope-Reducing Tibial Osteotomy Combined With Primary Anterior Cruciate Ligament Reconstruction Produces Improved Knee Stability in Patients With Steep Posterior Tibial Slope, Excessive Anterior Tibial Subluxation in Extension, and Chronic Meniscal Posterior Horn Tears. Am J Sports Med. 2020;48(14):3486-94.
-
27Su AW, Bogunovic L, Smith MV, et al. Medial Tibial Slope Determined by Plain Radiography Is Not Associated with Primary or Recurrent Anterior Cruciate Ligament Tears. J Knee Surg. 2020;33(1):22-8.
-
28Imhoff AB, Feucht M, Achtnich A, Imhoff F, Herbst E, Diermeier T. Three-dimensional realignment and slope reducing osteotomy with anatomic ACL reconstruction in patients with revision anterior cruciate ligament deficiency. Orthop J Sports Med. 2020;8(9 suppl):2325967120S00524.
-
29Zaffagnini S, Bonanzinga T, Grassi A, et al. Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc. 2013;21:934-41.
-
30Won HH, Chang CB, Je MS, Chang MJ, Kim TK. Coronal limb alignment and indications for high tibial osteotomy in patients undergoing revision ACL reconstruction. Clin Orthop Relat Res. 2013;471(11):3504-11.
-
31Schneider A, Gaillard R, Gunst S, et al. Combined ACL reconstruction and opening wedge high tibial osteotomy at 10-year follow-up: excellent laxity control but uncertain return to high level sport. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):960-8.
-
32Kim SJ, Moon HK, Chun YM, Chang WH, Kim SG. Is correctional osteotomy crucial in primary varus knees undergoing anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2011;469(5):1421-6.
-
33Jin C, Song EK, Jin QH, et al. Outcomes of simultaneous high tibial osteotomy and anterior cruciate ligament reconstruction in anterior cruciate ligament deficient knee with osteoarthritis. BMC Musculoskelet Disord. 2018;19:228.
-
34Trojani C, Elhor H, Carles M, Boileau P. Anterior cruciate ligament reconstruction combined with valgus high tibial osteotomy allows return to sports. Orthop Traumatol Surg Res. 2014;100:209-12.
-
35Schuster P, Schulz M, Richter J. Combined biplanar high tibial osteotomy, anterior cruciate ligament reconstruction, and abrasion/microfracture in severe medial osteoarthritis of unstable varus knees. Arthroscopy. 2016;32:283-92.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- We are living a golden age in Spanish arthroscopic surgery
- Alteration of the coronal and sagittal axes of the knee and its implication in the failure of anterior cruciate ligament reconstruction. A systematic review
- Arthroscopic acetabular microfractures of the hip: survival and clinical outcome of the technique with a minimum follow-up of 5 years
- Hip arthroscopy provides medical personnel with an early and complete return to work. A multicentre study
- Novel articles on combined ligamentous injury of the anterior cruciate ligament and medial ligament complex of the knee
- Anteroinferior shoulder instability. Essential articles
- Treatment of shoulder instability with bone defects using a combination of arthroscopic bone block and <em>remplissage</em> techniques
- Reconstruction of the rotator cuff using a triple-row arthroscopic technique. Surgical technique
- Endoscopic treatment of calcific tendinitis of the gluteus maximus. A case report
- Incomplete discoid medial meniscus presenting coalescence with the anterior cruciate ligament
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.