Results of the arthroscopic treatment of acute bony Bankart lesion using the original Porcellini-Sugaya technique and the double-row modified procedure
Resultados del tratamiento artroscópico del Bankart óseo agudo mediante técnica de Porcellini-Sugaya original y modificada en doble hilera
Resumen:
Objetivo: analizar los resultados obtenidos del tratamiento artroscópico de la lesión aguda de Bankart óseo, utilizando la técnica de Porcellini-Sugaya y su modificación en doble hilera.
Métodos: revisión retrospectiva de pacientes con diagnóstico de lesión aguda de Bankart óseo entre los años 2017 y 2022, intervenidos por vía artroscópica mediante 2 técnicas quirúrgicas, la técnica original Porcellini-Sugaya y la modificada en doble hilera. Se analizaron los tiempos quirúrgicos, el número de implantes utilizados, las complicaciones, el rango de movilidad activa al final del seguimiento, la escala de valoración clínica Disabilities of the Arm, Shoulder and Hand (DASH) y el tiempo de baja laboral.
Resultados: se revisaron 12 pacientes en un tiempo medio de seguimiento de 28 meses (6-50). Siete pacientes fueron intervenidos mediante la técnica convencional de Porcellini-Sugaya y 5 con la técnica modificada doble hilera/doble polea. En el grupo de Porcellini-Sugaya la puntuación media en la escala DASH fue de 2,6 (0-15) y en el grupo doble hilera/doble polea de 41,2 (21-69,7). La rotación externa fue el rango de movilidad postoperatorio más afectado en ambos grupos, siendo en el grupo de Porcellini-Sugaya de 71° (30-90) y de 44° (20-60) en el grupo de doble hilera. No hubo recidivas de luxación ni otras complicaciones.
Conclusiones: las técnicas artroscópicas de Porcellini-Sugaya y sus modificaciones son efectivas en el tratamiento de las lesiones de Bankart óseo agudo, obteniendo resultados similares en estabilidad y ausencia de recidiva.
Nivel de evidencia: estudio clínico, nivel de evidencia IV.
Relevancia clínica: el tratamiento artroscópico agudo de las lesiones de Bankart óseo es recomendable para evitar la inestabilidad que producen estas. Los resultados obtenidos de esta revisión pueden ser relevantes dada la escasa bibliografía actual presente, ofreciendo resultados actualizados que comparan 2 técnicas quirúrgicas artroscópicas de reciente descripción y poco frecuentes.
Abstract:
Objective: To analyse the results obtained with the arthroscopic treatment of acute bony Bankart lesion using the original Porcellini-Sugaya technique and the double-row modified procedure.
Methods: A retrospective analysis was made of patients diagnosed with acute bony Bankart lesion between the years 2017 and 2022, subjected to arthroscopic surgery using two surgical techniques: the original and the double-row modified Porcellini-Sugaya technique. Evaluation was made of the surgical times, the number of implants used, the complications, active range of motion at the end of follow-up, the Disabilities of the Arm, Shoulder and Hand (DASH) clinical score, and patient days off work.
Results: A total of 12 patients with a mean follow-up of 28 months (range 6-50) were evaluated. Seven patients were operated upon using the conventional Porcellini-Sugaya technique, and 5 were operated upon using the modified double-row / double pulley technique. In the Porcellini-Sugaya group, the mean DASH score was 2.6 (0-15), versus 41.2 (21-69.7) in the double-row / double pulley group. External rotation was the postoperative range of motion most affected in both groups, with 71° (30-90) in the Porcellini-Sugaya group and 44° (20-60) in the double-row group. There were no luxation relapses or other complications.
Conclusions: The arthroscopic techniques of Porcellini-Sugaya and its modifications are effective in treating acute bony Bankart lesion, affording similar outcomes in terms of stability, and with no relapses.
Level of evidence: Clinical study, level of evidence IV.
Clinical relevance: The arthroscopic treatment of acute bony Bankart lesions is advisable in order to avoid the instability they cause. The results obtained in this review may be relevant due to the scant existing literature, evidencing up-to-date results comparing two recently described and infrequent arthroscopic surgical techniques.
Introduction
Bony Bankart lesions are fractures of the anterior glenoid margin associated to avulsions of the labral capsular-ligament complex(1).
Direct trauma to the shoulder, with impacting of the humeral head in the glenoid cavity in some cases results in glenoid fracture and consequent glenohumeral dislocation. Glenoid bony lesions of this kind often evolve towards relapsing glenohumeral instability(1). When the size of the glenoid fracture proves relevant, with a classically established critical value of 20-25% of the area(2) and a currently defined value of 15% or more(3), surgery is the ideal treatment for avoiding the subsequent relapse of instability(4,5). Porcellini et al. in 2002(4) and Sugaya et al. in 2005(5) described the arthroscopic repair technique for lesions of this kind, consisting of reduction and block osteocapsular-ligamentous-labral fixation (Figure 1). Posteriorly, more sophisticated modifications of the technique were developed, such as the double-row / double pulley procedure of Ganokroj(6), consisting of a block reconstruction based on fixation at two different points: an anchoring medial with respect to the chondral margin of the glenoid cavity, and a lateral anchoring in the glenoid margin. Furthermore, other open and arthroscopic technical modifications have been described for such lesions(7).
The present study was carried out to analyse the outcomes obtained with the arthroscopic treatment of acute bony Bankart lesion, based on the comparison of two infrequent techniques for which few studies are currently available: the original Porcellini-Sugaya technique and the double pulley modified procedure of Ganokroj.
Methods
A retrospective review of a series of consecutive cases was made. The included patients presented a diagnosis of acute bony Bankart lesion (acute lesions being defined as those with an evolution of under 2 months) and with a bone fragment size > 15% of the total glenoid surface, produced in the patient work setting in the period 2017-2021, and subjected to arthroscopic surgery based on the conventional Porcellini-Sugaya technique and on the modified double-row / double pulley procedure ― with no other added surgical measures.
Patients with an over two-month-old bony Bankart lesion and a bone fragment size < 15% of the total glenoid surface were excluded. We also excluded those patients subjected to remplissage or other added surgical measures.
The minimum duration of follow-up was 6 months and the maximum 50 months. The criterion for using one surgical technique or the other was based on the preferences of the surgeon. The electronic medical records of the patients were reviewed, along with the images of the arthroscopic surgeries, and the patients were contacted by telephone. Data were obtained on the active range of motion of the shoulder contralateral to the lesion prior to surgery, the surgical times, the number of implants used, the complications, final active range of motion of the injured shoulder (antepulsion, abduction, external rotation and internal rotation), the Disabilities of the Arm, Shoulder and Hand (DASH) clinical score, and patient days off work.
The null hypothesis was the absence of differences between the two groups (Porcellini-Sugaya group and modified double-row group), while the alternative hypothesis was the existence of significant differences between the two groups.
Surgical procedure
All the patients were operated upon under general anaesthesia and interscalene plexus block. The patients were placed in lateral decubitus with traction, and the stability of both shoulders was explored. Instability of the damaged shoulder was confirmed in all cases. All patients were operated upon by the same two surgeons. No other surgical measures were adopted, except those related to osteocapsular-labral repair. The usual portals for arthroscopic surgery of instability were used: posterior and anterosuperior viewing portals and posterior, anterosuperior and anteroinferior working portals.
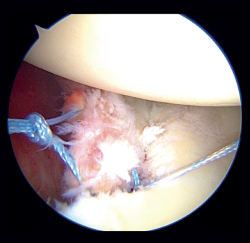
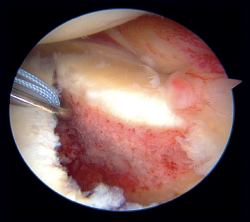
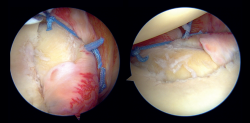
In the classical Porcellini-Sugaya technique, debridement and roughening of the bone margins of the fracture was carried out with synoviotome, rasps and curettes (Figure 2). All-suture anchorings were used for the repair. The first anchoring was placed in the lowermost zone of the defect (Figure 3), and one its extremities extended to the damaged labrum in the lowermost zone, followed by knotting. The second anchoring was placed in the uppermost zone of the defect (Figure 4), in the same way as the first, followed by knotting. In those cases where considered necessary, one or two more anchorings were added proximal to the previous ones. Reduction and stability of the fragment was checked.
reacae.30178.fs2207012-figure3.png
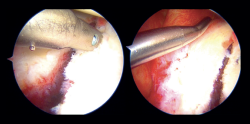
Figure 3. Arthroscopic view of a right shoulder. Position in left lateral decubitus. Anterosuperior vision portal. The image at left shows placement of the most distal implant in the classical Porcellini-Sugaya technique. The image at right shows passage of the suture through the anteroinferior labrum.
In the modified double-row/double pulley technique, and in addition to the measures commented above, an anchoring was added between the first implant and the second, at the height of half of the fractured bone fragment but in a position medial with respect to the chondral margin of the glenoid cavity (Figure 5). In this case, both the extremities crossed through the capsule at the level of half of the fragment and anterior to the latter at different points, followed by knotting and maintaining reduction of the bone fragment (Figure 6). One of the extremities of the suture knot made was tied to one of the extremities of the lower anchoring, while the other was tied to one of the extremities of the upper anchoring, thereby completing the repair procedure (Figure 7).
Postoperative protocol
The shoulder was immobilised with a conventional sling for four weeks. No active or passive mobilisation of the shoulder was allowed, though the elbow could be moved during that period of time. Passive rehabilitation exercises started from the fourth to the sixth week, and after this period assisted active work was started. Surgical wound cures were made on postoperative days 7 and 15 by the Nursing Department, and the first follow-up control by the supervising surgeon was performed after three weeks.
Statistical analysis
The descriptive and inferential analyses were made using the IBM SPSS statistical package. The Shapiro-Wilk test was used to establish the distribution of the variables (parametric or nonparametric). All variables except flexion and abduction followed a normal distribution. The results of the two groups (Porcellini-Sugaya group and modified double-row group) were compared using the Student t-test for all study variables, except flexion and abduction, where the Mann-Whitney U-test was used, and patient gender, where the chi-square test was used. Statistical significance was considered for p < 0.05.
reacae.30178.fs2207012-figure6.png
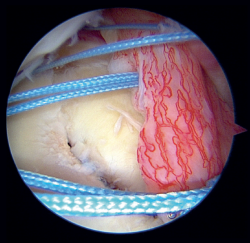
Figure 6. Arthroscopic view of a left shoulder. Position in right lateral decubitus. Anterosuperior vision portal. Note the sutures of the three anchorings (distal, central and proximal) after passing through the labrum and prior to final knotting in the modified double-row / double pulley technique.
Results
All of the operated patients were males. In 8 of the 12 patients, the episode of anterior glenohumeral dislocation was radiologically associated to the definitive diagnosis. Computed axial tomography (CAT) was performed in 11 patients prior to surgery, while magnetic resonance imaging (MRI) was performed in 10. The mean age was 43 years (range 30-65). There were no statistically significant differences between the two groups in terms of age or gender, with a homogeneous distribution between the Porcellini-Sugaya group and the double-row group. The right shoulder was the most affected shoulder (7 out of 12 patients). The mean duration of follow-up was 28 months (range 6-50), and the mean time from diagnosis of the lesion to surgery was 23 days. Evaluation was made of the preoperative stability and mobility of the shoulder contralateral to the lesion in order to establish a comparison versus the final outcome of the injured shoulder; all the patients presented a full range of motion and no instability.
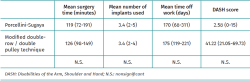
The mean global surgery time was 122 minutes (range 72-91). In the Porcellini-Sugaya group, the mean time was 119 minutes (range 72-191) versus 126 minutes (range 98-149) in the double-row group ― the difference being nonsignificant (p = 0.7). Likewise, there were no statistically significant differences in the number of implants used between the two groups, the total average being 3.4 implants (range 2-5). The mean days off work was 172 days (range 68-311). In the Porcellini-Sugaya group, the mean number of days was 170 (range 68-311) versus 175 days (range 119-221) in the double-row group ― the difference being nonsignificant (p = 0.78) (Table 1).
With regard to the functional and disability outcomes assessed with the DASH clinical scale, the mean score in the Porcellini-Sugaya group was 2.6 (range 0-15) versus 41.2 (range 21-69.7) in the double-row group ― the difference being nonsignificant (p = 0.25)(Table 1).
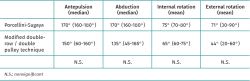
In relation to postoperative active range of motion, the median antepulsion range was 160º (60-180º); in the Porcellini-Sugaya group the range was 170º (160-180º) and in the double-row group the range was 150º (60-160º). In the case of abduction, the median total range was 167.5º (45-180°); in the Porcellini-Sugaya group the range was 170º (160-180°) and in the double-row group the range was 135° (45-165°). The total mean internal rotation range was 71° (60-80°); in the Porcellini-Sugaya group the range was 75° (70-80°) and in the double-row group the range was 65° (60-75°). Final external rotation yielded the poorest outcomes, with a median total range of 60° (20-90°); in the Porcellini-Sugaya group the range was 71° (30-90°) and in the double-row group the range was 44° (20-60°)(Table 2). There were no statistically significant differences between the two groups in terms of postoperative active range of motion referred to flexion (p = 0.21), abduction (p = 0.08), internal rotation (p = 0.18) or external rotation (p = 0.19).
None of the 12 reviewed patients presented dislocation relapse or apprehension at the end of follow-up. No infectious or neurovascular complications were recorded. Likewise, none of the patients presented signs of early-onset degenerative osteoarthrosis.
Discussion
The arthroscopic technique of Porcellini-Sugaya and its double-row / double pulley modification, which seek to secure reduction and stabilisation of the bone fragment, are effective in treating glenohumeral instability.
Porcellini et al.(4) published the outcomes of 25 patients with acute bony Bankart lesions presenting an evolution of under three months, affecting < 25% of the glenoid surface area, and operated upon using their arthroscopic technique. The 25 patients were evaluated over a minimum follow-up period of two years. None of the patients experienced recurrence of the dislocation. All the subjects reached complete antepulsion, and 8% of them suffered a decrease in external rotation. The postoperative clinical study evidenced no apprehension in any case. The postoperative radiographic evaluation showed correct healing of the bone fragment and the absence of pseudoarthrosis in 23 patients (92%). Sugaya et al.(5) in turn studied the outcomes of 8 patients with acute bony Bankart lesions presenting an evolution of under one month, and establishing a defect of > 20% as being relevant. None of the patients presented dislocation or instability, and all reported no apprehension. The CAT controls at 10 months evidenced no development of osteoarthrosis, and no cases of pseudoarthrosis were recorded. These results described first by Porcellini and subsequently by Sugaya are very similar to those obtained in our series in relation to the patients belonging to the Porcellini-Sugaya group, where none of the subjects presented recurrence of dislocation or instability, with good postoperative mobility.
Other authors have reported that repair techniques based on fixation at a single point, as in the Porcellini-Sugaya procedure, predispose the bone fragment to displacement in the direction of the implant, lessening reduction of the latter(8) and consequently affording poorer outcomes in terms of stability.
Young-Kyu et al.(9) evaluated 32 patients with acute bony Bankart lesion subjected to arthroscopic surgery based on a single fixation point, as in the Porcellini-Sugaya procedure, and documented residual joint incongruence in reduction with a displacement of > 2 mm in 22% of the treated cases. After one year of follow-up, these patients presented poorer functional outcomes, and two glenohumeral dislocation episodes were recorded, in discordance with our own findings in the Porcellini-Sugaya group.
Ganokroj et al.(6) described the modified double-row / double pulley technique and highlighted its advantages at surgical level, controlling tension during reduction of the fragment, and affording more stable and anatomical reduction due to greater fixation points. However, they reported no long-term clinical outcomes after surgery, and as a drawback pointed to the need for a greater learning curve versus other techniques(6). In order to compare our results obtained with the double-row / double pulley technique versus another similar series published in the literature, we found that Millet et al. described the bony Bankart bridge (BBB) technique, likewise based on fixation of the glenoid bone fragment at two different points in the medial-lateral direction. These authors placed an anchoring medial and another lateral to fix the bone fragment in a way similar to the transosseous double-row equivalent of a rotator cuff repair(10). In this regard, Godin et al.(11) described the outcomes in 13 patients with acute bony Bankart lesion subjected to the arthroscopic BBB technique, with a minimum follow-up of 5 years. The Quick-DASH clinical score was 6.2 (range 0-25). Of the 13 patients, three reported subjective instability sensation, though repeat surgery was not needed. Patient satisfaction was scored 10/10. Thus, the described technique based on fixation of the glenoid bone fragment at two different points, successfully restores shoulder stability. Millet et al.(12) analysed 15 patients with acute and chronic bony Bankart lesion treated with the BBB technique. The postoperative range of motion was 168° for antepulsion and 70° for external rotation, versus 124° and 44°, respectively, in our double-row group, with poorer outcomes in terms of joint range being noted in our series. The Quick-DASH clinical score was 2.8 (range 0-15.9), which is a favourable outcome in comparison with our double-row group. A single postoperative dislocation episode was recorded following direct trauma to the shoulder.
Atala et al.(8) described an arthroscopic technique based on fixation of the glenoid bone fragment at two different points for treating acute bony Bankart lesions, using two implants at medial level of the glenoid neck (one upper and the other lower), achieving fixation and final reduction with an implant preloaded from the sutures of the previous implants, after these passed through the capsuloligamentous-labral complex at the height of the glenoid joint surface at the margin of the fracture. The authors defended that with this technique the sutures do not traverse the two bone surfaces, affording great contact between them and producing better compression and rotation control of the fragment. The investigators reported that the greatest conflict with this procedure is its technical difficulty, and that performing it in lateral decubitus allows better visualisation, thereby facilitating surgery. However, the article did not evaluate long-term clinical outcomes with which to establish comparisons versus our own study.
Spiegl et al.(13) examined the results obtained in 14 pairs of glenoid cavities from paired cadavers with simulated bony Bankart fractures. Half of the fractures were repaired using the Porcellini-Sugaya technique, while the contralateral glenoid cavities were subjected to the double-row procedure. This study evidenced improvement in reduction and stability of the fracture when using the double-row technique versus repair with the conventional Porcellini-Sugaya technique.
On the basis of our findings and the data commented above, the Porcellini-Sugaya technique and its modifications are effective in treating acute bony Bankart lesion, in terms of stability and the recovery of joint range. No clinical studies comparing these techniques are currently available. The present study, which compares two infrequent arthroscopic techniques, seeks to offer improved knowledge of the outcomes obtained. The more complex and sophisticated modified double-row / double pulley technique, in search of theoretically improved stability and better anatomical reduction of the fractured glenoid fragments, in our series evidences a notable loss of joint range that must be assessed in future studies, in order to more precisely define its indications of use.
The main limitations of the present study are the limited sample size involved, its retrospective design, and the inclusion of patients in the work setting, where subjective and objective assessments are usually biased.
Conclusions
The arthroscopic techniques of Porcellini-Sugaya and its modifications are effective in treating acute bony Bankart lesion, affording good clinical outcomes and glenohumeral stability.
Figuras
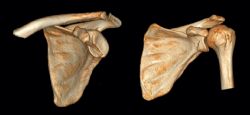
Figure 1. Computed tomography view, 3D reconstruction. Left: acute fracture of the anterior glenoid margin; right: the fracture, reduced and consolidated two years later.
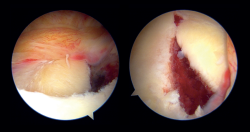
Figure 2. Arthroscopic view of a left shoulder with a bony Bankart lesion. Position in right lateral decubitus. From the posterior vision portal in the image at left, and from the anterosuperior vision portal in the image at right.
Figure 3. Arthroscopic view of a right shoulder. Position in left lateral decubitus. Anterosuperior vision portal. The image at left shows placement of the most distal implant in the classical Porcellini-Sugaya technique. The image at right shows passage of the suture through the anteroinferior labrum.
Figure 4. Arthroscopic view of a right shoulder. Position in left lateral decubitus. Anterosuperior vision portal. Fixation of the proximal implant in the classical Porcellini-Sugaya technique.
Figure 5. Arthroscopic view of a left shoulder. Position in right lateral decubitus. Anterosuperior vision portal. Central positioning, in the medial zone of the glenoid neck, of an anchoring in the modified double-row / double pulley technique.
Figure 6. Arthroscopic view of a left shoulder. Position in right lateral decubitus. Anterosuperior vision portal. Note the sutures of the three anchorings (distal, central and proximal) after passing through the labrum and prior to final knotting in the modified double-row / double pulley technique.
Figure 7. Arthroscopic view of a left shoulder. Position in right lateral decubitus. Modified double-row / double pulley technique. Final outcome of the repair. The image at left it is seen from the anterosuperior port. In the image at right it is seen from the posterior visioning portal.
Tablas
Información del artículo
Cita bibliográfica
Autores
Cristina Fernández Gallego
Complejo Asistencial Universitario de Salamanca
Santos Moros Marco
Servicio de Traumatología. Hospital MAZ. Zaragoza
Cirugía Ortopédica y Traumatología. Unidad de Miembro Superior. Hospital MAZ Zaragoza. Arthrosport Zaragoza
Editor asociado de REACA
Servicio de Traumatología y Cirugía Ortopédica. Hospital de la Mutua MAZ. Zaragoza
José Manuel García Pequerul
Servicio de Cirugía Ortopédica y Traumatología. Hospital MAZ Zaragoza
Unidad de Cirugía de Hombro y Codo. Servicio de Traumatología. Hospital MAZ. Zaragoza
José Luis Ávila Lafuente
Unidad de Cirugía de Hombro y Codo. Servicio de Traumatología. Hospital MAZ. Zaragoza
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed, and that all the patients included in the study have received sufficient information and have given written informed consent to participation in the study.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Nolte PC, Elrick BP, Bernholt DL, Lacheta L, Millett PJ. The Bony Bankart: Clinical and Technical Considerations. Sports Med Arthrosc Rev. 2020 Dec;28(4):146-52.
-
2Yamamoto N, Muraki T, An K, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013 Aug 7;95(15):1390-7.
-
3Shin S, Koh Y, Bui C, et al. What Is the Critical Value of Glenoid Bone Loss at Which Soft Tissue Bankart Repair Does Not Restore Glenohumeral Translation, Restricts Range of Motion, and Leads to Abnormal Humeral Head Position? Am J Sports Med. 2016 Nov;44(11):2784-91.
-
4Porcellini G, Campi F, Paladini P. Arthroscopic approach to acute bony Bankart lesion. Arthroscopy. 2002 Sep;18(7):764-9.
-
5Sugaya H, Kon Y, Tsuchiya A. Arthroscopic repair of glenoid fractures using suture anchors. Arthroscopy. 2005 May;21(5):635.
-
6Ganokroj P, Keyurapan E. Arthroscopic Bony Bankart Repair Using a Double-Row Double-Pulley Technique. Arthrosc Tech. 2018 Dec 10;8(1):e31-e36.
-
7Seidl AJ, Joyce CD. Acute Fractures of the Glenoid. J Am Acad Orthop Surg. 2020 Nov 15;28(22):e978-e987.
-
8Atala NA, Bongiovanni S, Rossi LA, et al. Arthroscopic Acute Bony Bankart Repair in Lateral Decubitus. Arthrosc Tech. 2020 Dec 21;9(12):e1907-e1915.
-
9Kim YK, Cho SH, Son WS, Moon SH. Arthroscopic repair of small and medium-sized bony Bankart lesions. Am J Sports Med. 2014 Jan;42(1):86-94.
-
10Millett PJ, Braun S. The "bony Bankart bridge" procedure: a new arthroscopic technique for reduction and internal fixation of a bony Bankart lesion. Arthroscopy. 2009 Jan;25(1):102-5.
-
11Godin J, Altintas B, Horan M, et al. Midterm Results of the Bony Bankart Bridge Technique for the Treatment of Bony Bankart Lesions. Am J Sports Med. 2019 Jan;47(1):158-64.
-
12Millett PJ, Horan MP, Martetschläger F. The "bony Bankart bridge" technique for restoration of anterior shoulder stability. Am J Sports Med. 2013 Mar;41(3):608-14.
-
13Spiegl UJ, Smith SD, Todd JN, Coatney GA, Wijdicks CA, Millett PJ. Biomechanical Comparison of Arthroscopic Single- and Double-Row Repair Techniques for Acute Bony Bankart Lesions. Am J Sports Med. 2014 Aug;42(8):1939-46.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- The COVID hangover
- Results of the arthroscopic treatment of acute bony Bankart lesion using the original Porcellini-Sugaya technique and the double-row modified procedure
- Assessment of tibial translation in experimental models of anterior cruciate ligament reconstructions: is dual tibial fixation indicated?
- Learning curve in the arthroscopic Latarjet technique
- Clinical outcomes of the anteromedial technique versus the transtibial technique in reconstruction of the anterior cruciate ligament: a systematic review and meta-analysis of randomized clinical trials
- Basic sciences in reconstruction of the anterior cruciate ligament with the ischiotibial tendons (a narrative review)
- Arthroscopic hip surgery in femoroacetabular impingement
- Circumferential 270º reconstruction of the hip labrum through arthroscopy with knotless tensionable technology Surgical technique
- Arthroscopic capsule reconstruction with dermal mesh plus segmental labral reconstruction with tibialis anterior allograft in recurrent postsurgical hip microinstability
- Synthetic polyethylene mesh augmentation for chronic patellar tendon rupture repair
- The Giant’s Causeway “inside the shoulder”
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.