Clinical outcomes of the anteromedial technique versus the transtibial technique in reconstruction of the anterior cruciate ligament: a systematic review and meta-analysis of randomized clinical trials
Resultados clínicos de la técnica anteromedial versus la técnica transtibial en la reconstrucción del ligamento cruzado anterior: revisión sistemática y metaanálisis de ensayos clínicos aleatorizados
Resumen:
Objetivo: comparar la técnica anteromedial versus la técnica transtibial para la realización del túnel femoral en la reconstrucción del ligamento cruzado anterior, con el fin de valorar si hay diferencias clínicas.
Métodos: revisión sistemática de ensayos clínicos aleatorizados que comparen los resultados clínicos de la técnica anteromedial versus la técnica transtibial en la reconstrucción del ligamento cruzado anterior. Se analizaron las variables demográficas, clínicas y quirúrgicas, incluyendo tipo de injerto, escalas funcionales y complicaciones.
Resultados: 9 ensayos clínicos aleatorizados fueron seleccionados. Se analizaron 763 pacientes: 386 pacientes (50,6%) operados mediante la técnica anteromedial y 377 pacientes (49,4%) operados mediante la técnica transtibial. Los resultados posquirúrgicos agrupados no encontraron diferencias significativas entre ambas técnicas en cuanto a la puntuación de Lysholm (p = 0,06), ni a la escala del International Knee Documentation Committee (IKDC) (p = 0,23), ni a la puntuación de Tegner (p = 0,97). Tampoco se encontraron diferencias en el número de complicaciones postoperatorias (p = 0,42), ni en el número de reintervenciones (p = 0,93).
Conclusiones: la técnica anteromedial y la transtibial en la reconstrucción del ligamento cruzado anterior tienen resultados clínicos equivalentes. No se observaron diferencias significativas entre ambas técnicas con respecto a las escalas funcionales, ni en cuanto a las complicaciones postoperatorias, ni en el número de reintervenciones.
Nivel de evidencia: 2.
Relevancia clínica: según los hallazgos obtenidos en el presente trabajo, para la reconstrucción del ligamento cruzado anterior realizar el túnel femoral mediante la técnica anteromedial o transtibial no tendría diferencias clínicas, en cuento a escalas funcionales, ni con respecto a complicaciones postoperatorias, ni en el número de reintervenciones, pudiendo optarse por una u otra según la preferencia del cirujano.
Abstract:
Objective: To compare the anteromedial technique versus the transtibial technique in performing the femoral tunnel in reconstruction of the anterior cruciate ligament, with a view to identifying possible clinical differences.
Methods: A systematic review was carried out of randomized clinical trials comparing the clinical outcomes of the anteromedial technique versus the transtibial technique in reconstruction of the anterior cruciate ligament. Demographic, clinical and surgical variables were analyzed, including the type of graft, functional scales and complications.
Results: Nine randomized clinical trials were selected. A total of 763 patients were analyzed: 386 (50.6%) were subjected to the anteromedial technique and 377 (49.4%) to the transtibial technique. The grouped postoperative outcomes revealed no significant differences between the two techniques in terms of the Lysholm score (p = 0.06), the International Knee Documentation Committee (IKDC) score (p = 0.23), or the Tegner score (p = 0.97). Likewise, there were no differences in the number of postoperative complications (p=0.42) or in the number of reoperations (p = 0.93).
Conclusions: The anteromedial technique and the transtibial technique in reconstruction of the anterior cruciate ligament result in equivalent clinical outcomes. No significant differences were observed between the two techniques in relation to the functional scales, postoperative complications or number of reoperations.
Level of evidence: 2.
Clinical relevance: Based on the findings of this study, performing the femoral tunnel for reconstruction of the anterior cruciate ligament using the anteromedial or the transtibial technique would not result in clinical differences in relation to the functional scales, postoperative complications or number of reoperations. The decision to use one technique or the other thus may be based on surgeon preference.
Introduction
Rupture of the anterior cruciate ligament (ACL) is the most frequent surgical ligament injury of the knee(1). The incidence is 36.9 surgical cases per 100,000 inhabitants/year, and the disorder poses an important economic, healthcare and occupational impact for every operation made, since most of these lesions occur in young individuals(1,2). Although the injury in most cases occurs during sports activity, ACL rupture usually causes instability and limitation in both the sports and the daily life setting(3). For this reason, and because of the high prevalence of injuries of this kind, it is crucial to repair them with the best possible treatment in order to secure a knee with the same functional capacity as before the lesion(4).
Correct reconstruction of the ACL in terms of native dimensions, orientation and points of insertion is of vital importance, since it allows more precise restoration of the knee kinematics and improves the long term outcome(5). The short term aim of reconstruction of the ACL is to restore knee stability and thus improve the patient symptoms. The fundamental long term aim is to avoid degenerative changes of the joint(6). Reconstruction at femoral level has evolved over time. In 2006, the transtibial technique (TT), with the concept of plasty isometry, in which only a single tunnel was made, constituted the most widely used ACL reconstruction procedure(7). However, a number of studies raised concern about possible failure of the reconstruction due to the non-anatomical placement of the ligament(5,8). The anteromedial technique (AM) mainly seeks anatomical placement of the plasty in the insertion footprint of the ACL at femoral level. It is a more recent technique and one of the current trends in reconstruction of the ACL(9). The most recent surveys, published in 2013 and 2015, found that 68% of the surgeons currently use an independent perforation procedure, the AM technique, while only 31% still use a TT guide(10,11). Nevertheless, the AM technique is not without potential complications, including the risk of rupture or damage to the lateral structures (iliotibial band, plantaris muscle, lateral gastrocnemius or common peroneal nerve), damage of the internal femoral condyle, or the creation of excessively short femoral tunnels(12,13). Important controversy remains as to which of the two techniques, AM or TT, affords the best outcomes in reconstruction of the ACL.
With the hypothesis that the AM technique offers better functional outcomes, with fewer postoperative complications and a lesser reintervention risk than the TT technique, the present study was carried out to compare AM versus TT for creating the femoral tunnel in reconstruction of the ACL, based on a systematic review of randomized clinical trials (RCTs).
Methods
Systematic literature review
The systematic review was based on the Cochrane review and abided with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. A literature search was carried out in the PubMed database (https://pubmed.ncbi.nlm.nih.gov/). The electronic search was carried out between July and September 2022. We considered studies published up until 15 September 2022 that evaluated the clinical outcomes in patients subjected to reconstruction of the ACL using the AM or the TT technique. The search terms in English were: 1) “anterior cruciate ligament reconstruction” o “ACL reconstruction”; 2) “transtibial” o “conventional”; 3) “anteromedial” o “anatomical” o “transportal”; 4) “randomized controlled trials” or “RCT”.
Inclusion and exclusion criteria
The following study inclusion criteria were applied: 1) RCTs; 2) studies involving patients subjected to primary arthroscopic surgery of the ACL and which compared AM versus TT; 3) studies reporting complete data, including sample number per group, mean and standard deviation (SD); 4) studies clinically assessing the postsurgical outcomes of the two techniques based on validated knee scales; and 5) studies evaluating postoperative complications and the need for repeat surgery. Those studies meeting the following criteria were excluded from the analysis: 1) studies in cadavers; 2) studies failing to report postsurgical outcomes based on means with SD or percentages; 3) studies without full text in English; and 4) studies involving duplicate data.
Selection of studies
The titles and abstracts of the articles generated by the search were evaluated, and the relevant publications were selected for full-text review. If the abstract did not provide enough information to make a decision, the full-text article was reviewed. We also performed manual searches for articles potentially omitted by the electronic search. On analyzing and organizing the studies, we assessed the country and the hospital or institution where the surgeries were performed, the name of the surgeon in the studies and the evaluation period, in order to identify duplicate patient cohorts. If the same patient cohort was evaluated in more than one study, we included the latest study with the longest follow-up period, and excluded the rest. Following the PRISMA guidelines, two independent reviewers (A.P. and J.H.N.) evaluated the titles, abstracts and full-text articles. In the case of debate regarding the inclusion of an article, a third independent reviewer (E.G.) was consulted.
Study variables
Two investigators independently extracted the data from the studies included in the final analysis. A predefined data extraction form was used. Any unresolved disagreement between the two investigators was reviewed by a third investigator (E.G.). The demographic variables included patient age (years) at the time of surgery, gender (male/female), time between injury and surgery (weeks), and follow-up time (months). On the other hand, the collected clinical variables included the International Knee Documentation Committee (IKDC) score, the Lysholm knee score and the Tegner activity scale(14). Lastly, we recorded the following surgical variables: postoperative complications and need for repeat surgery.
Quality assessment
The quality of the RCTs was assessed using Review Manager (RevMan) version 5.3 (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, 2014), in order to assess risk of bias. The evaluation methods involved the following steps: random sequence generation, concealment of allocation, blinding, incomplete outcome data, and selective outcome reporting. The scores in these domains were entered in a general risk of bias evaluation for a given RCT: I) “low risk of bias”; II) “some concerns”; or III) “high risk of bias”.
Statistical analysis
A descriptive analysis was made, with the reporting of means and SD for continuous variables, and absolute frequencies and percentages for categorical variables. The meta-analysis was carried out with RevMan (version 5.3) of the Cochrane community. In the case of binary variables we used the odds ratio (OR) for evaluation, while in the case of continuous variables we employed the standardized mean difference (SMD), with a 95% confidence interval (CI). The heterogeneity of the studies was assessed with the I2 test. The inverse variance random effects model was applied. Statistical significance was considered for p < 0.05.
Results
Literature review
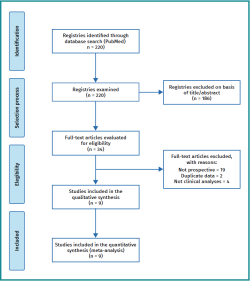
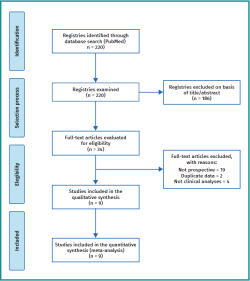
The initial search yielded a total of 220 studies, of which 186 were excluded from the systematic review after reading the title and/or abstract. After review of the full text of the remaining 34 studies, a total of 25 were excluded, leaving 9 RCTs for inclusion in the final analysis(15-23) (Figure 1). Figure 2 summarizes the risk of bias.
Characteristics of the studies
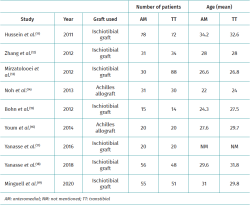
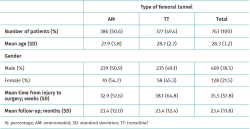
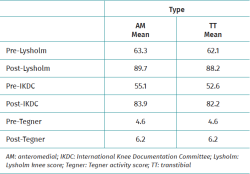
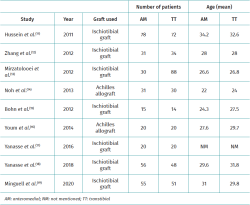
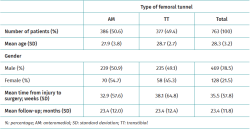
The characteristics of each study are reported in Table 1. The meta-analysis included a total of 763 patients, of which 386 (50.6%) and 377 (49.9%) were subjected to reconstruction of the ACL using the AM technique and the TT technique, respectively. The global mean age was 28.3 years (SD: 3.2)(15,16,17,18,19,20,22,23). The mean age was 28.1 years (SD: 2.9) in the case of the AM technique and 29.7 years (SD: 1.7) in the case of the TT technique, with no statistically significant differences between them (SMD: −0.10; 95%CI: −0.34-0.13; p = 0.40)(19,20,22,23). Gender was mentioned in 7 of the studies. There were 234 males and 70 females in the case of the AM technique and 235 males and 58 females in the case of the TT technique, with no statistically significant differences between the two (OR: 0.84; 95%CI: 0.55-1.29; p = 0.43)(19,20,22,23). Seven studies used autologous ischiotibial grafts (77.7%)(15,16,17,19,21,22,23), while the remaining two used graft material from a tissue bank(18,20). The time between injury and surgery was only reported in 5 studies, the average being 35.5 weeks. However, on excluding the study of Minguell et al.(23) from the analysis, the mean time between injury and surgery was reduced to 8.2 weeks (SD: 2.2). Lastly, the mean follow-up period of the patients was 23.4 months (range: 12-52; SD: 11.8) (Table 2).
Clinical outcomes
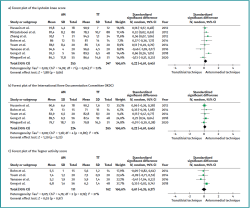
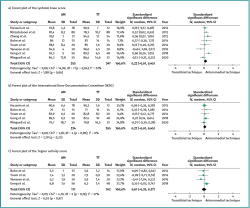
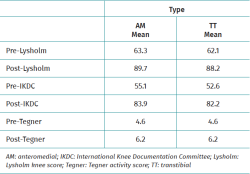
The most frequently used scales, in decreasing order, were the Lysholm, IKDC and Tegner scales. Seven studies reported at least two functional scales(15,17,20,21,22,23) and only one(19) reported all three functional scales (Table 3). There were no statistically significant differences in terms of the best outcomes with the AM technique according to the Lysholm score (SMD: 0.22; 95%CI: −0.01-0.45; p = 0.06), with moderate heterogeneity (I2: 53%; p = 0.04), versus the IKDC scale (SMD: 0.12; 95%CI: −0.07-0.31; p = 0.23), with null heterogeneity (I2: 0%; p = 0.85), or versus the Tegner scale (SMD: 0.01; 95%CI: −0.35-0.37; p = 0.97), with moderate heterogeneity (I2: 37%; p = 0.19) (Figure 3).
Surgical outcomes
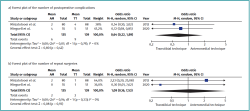
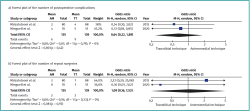
Only two studies, comprising 274 patients, reported the number of postoperative complications and the number of repeat surgeries(17,23). There were no differences in the number of postoperative complications between the AM technique (4.4%) and the TT technique (6.5%)(OR: 0.64; 95%CI: 0.22-1.89; p = 0.42), with null heterogeneity (I2: 0%; p = 0.79). Likewise, there were no differences in the number of repeat surgeries between the AM technique (1.5%) and the TT technique (1.4%)(OR: 1.09; 95%CI: 0.16-7.53; p = 0.93), with null heterogeneity (I2: 0%; p = 0.33) (Figure 4).
Discussion
The main finding of this study was the absence of significant clinical differences in terms of the functional scales, postoperative complications or number of repeat surgeries between the AM technique and the TT technique in the reviewed RCTs.
With regard to patient age (p = 0.40) and gender (p = 0.43), no statistically significant differences were observed between the two techniques. This is important because it can limit demographic bias. In relation to the clinical outcomes, no significant differences were observed between the AM and TT techniques in terms of the functional scales used (Tegner, Lysholm and IKDC). It must be noted that only two RCTs reported a clinical difference between the two techniques(17,18). Mirzatolooei et al. recorded better clinical outcomes at short term in reference to both the IKDC and the Lysholm scores, in favor of the AM technique(17). Likewise, Noh et al. reported statistically significant differences with the Lysholm score (p < 0.025) in favor of the AM group. However, they found no significant differences in the IKDC or Tegner scores (p > 0.05) on comparing the two groups(18). The rest of the 7 RCTs analyzed reported no clinical differences according to the functional scores(15,16,19,20,21,22,23). These discrepancies also appear in old meta-analyses. In their meta-analysis, Liu et al. recorded higher Lysholm scores (p = 0.034) and a greater incidence of grade A/B with IKDC (p = 0.04) on using the AM technique versus the TT procedure(24). Ro et al. found that the proportion of patients with normal grades according to IKDC (p = 0.0006) and the Lysholm score (p = 0.02) after surgery was greater with AM than with TT, though there were no differences in the total IKDC and Tegner scores(25). Chen et al. observed no differences in patient-reported functional outcome (Lysholm score), but did find differences in the objective IKDC score recorded by the surgeon, in favor of the AM technique(26). It must be noted that these latter meta-analyses also included nonrandomized prospective and retrospective studies(24,25,26). Considering all these data and our results, it can be concluded that either technique, when adequately performed, can afford sufficient knee stability to allow the patient to develop his or her sports activities, with no clinically relevant differences between the two procedures(20).
There were no significant differences in terms of postoperative complications or in the number of reoperations on comparing both techniques. These results are consistent with those of previous studies such as the meta-analysis carried out by Chen et al., where the differences likewise failed to reach statistical significance (p > 0.05)(27). However, only two studies reported these variables(17,18,19,20,21,22,23). Mirzatolooei et al. reported three saphenous nerve injuries with resulting dysesthesia on the anteromedial surface of the leg in the TT group and two in the AM group. One case of septic arthritis was documented in the TT group(17). Minguell et al. found both techniques to present a similar plasty failure rate one year after surgery, with a total of 9 graft failures (8.57%): four in the AM group and 5 in the TT group(23).
As can be seen from this literature review, there is still much controversy regarding the existence of relevant differences between the two techniques. In this regard, consideration is also required of a number of limitations of the present study. Firstly, few studies were included in the analysis, which may imply insufficient evidence. Nevertheless, we only included RCTs, which is a strength of our meta-analysis. Secondly, some results have moderate heterogeneity, which may introduce bias in our study in relation to the Lysholm score (I2: 53%; p = 0.04) and the Tegner score (I2: 37%; p = 0.19).
Another limitation of the systematic review is the relatively short follow-up in the included studies, with only two articles reporting follow-up periods of over two years. We therefore consider it to be particularly relevant to carry out long-term studies to assess the clinical impact of longer time intervals. Another important limitation is the scant recording of complications and of the need for repeat surgery, which may be important variables for deciding to use one technique or the other(13,19).
Conclusions
In reconstruction of the ACL, performing the femoral tunnel with the AM or the TT technique results in similar clinical outcomes. No significant differences were observed between the two techniques in relation to the functional scales, postoperative complications or number of reoperations.
Figuras
Figure 1. Flowchart of the identification and selection of the studies included in the present systematic review.
Figure 2. Summary of risk of bias. Green: “low risk of bias”; red: “high risk of bias”; yellow: “uncertain risk of bias”.
Figure 3. 95%CI: 95% confidence interval; AM: anteromedial technique; SD: standard deviation; TT: transtibial technique.
Figure 4. 95%CI: 95% confidence interval; AM: anteromedial technique; OR: odds ratio; TT: transtibial technique.
Tablas
Información del artículo
Cita bibliográfica
Autores
Aleix Pons Bartolí
Artroesport. Cirugía Ortopédica y Traumatología. Centro Médico Teknon. Grupo Quirón Salud. Barcelona
Cirugía Ortopédica y Traumatología. Grupo Quirón Salud. Hospital Quirónsalud Barcelona
Instituto Cugat. Quirónsalud Barcelona
Kushal Lakhani
Cirugía Ortopédica y Traumatología. Universitat Autònoma de Barcelona
Hospital Universitari Vall d’Hebron. Barcelona
Judith Martínez Peñas
Cirugía Ortopédica y Traumatología. Universitat de Barcelona
Hospital Universitario Mutua de Terrassa. Barcelona
Ernesto Guerra Farfan
Artroesport. Cirugía Ortopédica y Traumatología. Centro Médico Teknon. Grupo Quirón Salud. Barcelona
Servicio de Cirugía Ortopédica y Traumatología. Unidad de Tobillo y Pie. Hospital Universitari Vall d’Hebron. Barcelona
Osvaldo Gómez
Artroesport. Cirugía Ortopédica y Traumatología. Centro Médico Teknon. Grupo Quirón Salud. Barcelona
Antoni Fraguas
Artroesport. Cirugía Ortopédica y Traumatología. Centro Médico Teknon. Grupo Quirón Salud. Barcelona
Jorge H. Núñez
Artroesport. Cirugía Ortopédica y Traumatología. Centro Médico Teknon. Grupo Quirón Salud. Barcelona
Cirugía Ortopédica y Traumatología. Universitat de Barcelona
Hospital Universitario Mutua de Terrassa. Barcelona
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport. 2009;12:622-7.
-
2Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-Specific Yearly Risk and Incidence of Anterior Cruciate Ligament Tears in High School Athletes: A Systematic Review and Meta-analysis. Am J Sports Med. 2016;44:2716-23.
-
3Kobayashi H, Kanamura T, Koshida S, et al. Mechanisms of the anterior cruciate ligament injury in sports activities: a twenty-year clinical research of 1,700 athletes. J Sport Sci Med. 2010;9:669-75.
-
4Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between Objective Assessment of Ligament Stability and Subjective Assessment of Symptoms and Function after Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2004;32:629-34.
-
5Fu FH, Karlsson J. A long journey to be anatomic. Knee Surg Sports Traumatol Arthrosc. 2010 Sep;18(9):1151-3.
-
6Bergerson E, Persson K, Svantesson E, et al. Superior Outcome of Early ACL Reconstruction versus Initial Non-reconstructive Treatment With Late Crossover to Surgery: A Study From the Swedish National Knee Ligament Registry. Am J Sports Med. 2022;50:896-903.
-
7Duquin TR, Wind WM, Fineberg MS, Smolinski RJ, Buyea CM. Current trends in anterior cruciate ligament reconstruction. J Knee Surg. 2009;22:7-12.
-
8Franceschi F, Papalia R, Rizzello G, Del Buono A, Maffulli N, Denaro V. Anteromedial portal versus transtibial drilling techniques in anterior cruciate ligament reconstruction: any clinical relevance? A retrospective comparative study. Arthroscopy. 2013;29:1330-7.
-
9Hwang MD, Piefer JW, Lubowitz JH. Anterior cruciate ligament tibial footprint anatomy: systematic review of the 21st century literature. Arthroscopy. 2012 May;28(5):728-34.
-
10Kim HS, Seon JK, Jo AR. Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2013 Dec;25(4):165-73.
-
11Vaishya R, Agarwal AK, Ingole S, Vijay V. Current trend in anterior Anterior Cruciate Ligament Reconstruction: A Review. Cureus. 2015;(7)11:e378.
-
12Rhatomy S, Yudhistira JF, Soekarno NR, Setyawan R. Iatrogenic injury of posterolateral structures during femoral tunneling in anterior cruciate ligament reconstruction: a cadaveric study. Ann Med Surg (Lond). 2020;59:14-6.
-
13Hall MP, Ryzewicz M, Walsh PJ, Sherman OH. Risk of iatrogenic injury to the peroneal nerve during posterolateral femoral tunnel placement in double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:109-13.
-
14Kocher MS, Steadman JR, Briggs K, et al. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84-A:1560-72.
-
15Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med. 2012 Mar;40(3):512-20.
-
16Zhang Q, Zhang S, Li R, Liu Y, Cao X. Comparison of two methods of femoral tunnel preparation in single-bundle anterior cruciate ligament reconstruction: a prospective randomized study. Acta Cir Bras. 2012 Aug;27(8):572-6.
-
17Mirzatolooei F. Comparison of short term clinical outcomes between transtibial and transportal TransFix® femoral fixation in hamstring ACL reconstruction. Acta Orthop Traumatol Turc. 2012;46(5):361-6.
-
18Noh JH, Roh YH, Yang BG, Yi SR, Lee SY. Femoral tunnel position on conventional magnetic resonance imaging after anterior cruciate ligament reconstruction in young men: transtibial technique versus anteromedial portal technique. Arthroscopy. 2013 May;29(5):882-90.
-
19Bohn MB, Sørensen H, Petersen MK, Søballe K, Lind M. Rotational laxity after anatomical ACL reconstruction measured by 3-D motion analysis: a prospective randomized clinical trial comparing anatomic and nonanatomic ACL reconstruction techniques. Knee Surg Sports Traumatol Arthrosc. 2015 Dec;23(12):3473-81.
-
20Youm YS, Cho SD, Lee SH, Youn CH. Modified transtibial versus anteromedial portal technique in anatomic single-bundle anterior cruciate ligament reconstruction: comparison of femoral tunnel position and clinical results. Am J Sports Med. 2014 Dec;42(12):2941-7.
-
21Yanasse RH, Lima AA, Antoniassi RS, et al. Transtibial technique versus two incisions in anterior cruciate ligament reconstruction: tunnel positioning, isometricity and functional evaluation. Rev Bras Ortop. 2016;51:274-81.
-
22Geng Y, Gai P. Comparison of 2 femoral tunnel drilling techniques in anterior cruciate ligament reconstruction. A prospective randomized comparative study. BMC Musculoskelet Disord. 2018;19:1-7.
-
23Minguell J, Núñez JH, Reverte-Vinaixa MM, Sallent A, Gargallo-Margarit A, Castellet E. Femoral tunnel position in chronic anterior cruciate ligament rupture reconstruction: randomized controlled trial comparing anatomic, biomechanical and clinical outcomes. Eur J Orthop Surg Traumatol. 2019;29:1501-9.
-
24Liu A, Sun M, Ma C, et al. Clinical outcomes of transtibial versus anteromedial drilling techniques to prepare the femoral tunnel during anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25:2751-9.
-
25Ro KH, Kim HJ, Lee DH. The transportal technique shows better clinical results than the transtibial techniques for single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:2371-80.
-
26Chen Y, Chua KH, Singh A, et al. Outcome of Single-Bundle Hamstring Anterior Cruciate Ligament Reconstruction Using the Anteromedial Versus the Transtibial Technique: A Systematic Review and Meta-analysis. Arthroscopy. 2015;31:1784-94.
-
27Chen H, Tie K, Qi Y, Li B, Chen B, Chen L. Anteromedial versus transtibial technique in single-bundle autologous hamstring ACL reconstruction: a meta-analysis of prospective randomized controlled trials. J Orthop Surg Res. 2017;12:167.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- The COVID hangover
- Results of the arthroscopic treatment of acute bony Bankart lesion using the original Porcellini-Sugaya technique and the double-row modified procedure
- Assessment of tibial translation in experimental models of anterior cruciate ligament reconstructions: is dual tibial fixation indicated?
- Learning curve in the arthroscopic Latarjet technique
- Clinical outcomes of the anteromedial technique versus the transtibial technique in reconstruction of the anterior cruciate ligament: a systematic review and meta-analysis of randomized clinical trials
- Basic sciences in reconstruction of the anterior cruciate ligament with the ischiotibial tendons (a narrative review)
- Arthroscopic hip surgery in femoroacetabular impingement
- Circumferential 270º reconstruction of the hip labrum through arthroscopy with knotless tensionable technology Surgical technique
- Arthroscopic capsule reconstruction with dermal mesh plus segmental labral reconstruction with tibialis anterior allograft in recurrent postsurgical hip microinstability
- Synthetic polyethylene mesh augmentation for chronic patellar tendon rupture repair
- The Giant’s Causeway “inside the shoulder”
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.