Introduction
Patellar tendon rupture is considered to be an infrequent injury that causes knee extension disability. Its incidence is greatest in males between the third and fourth decades of life. It is relatively common for such lesions to go undetected in a first visit, with progression towards chronicity in up to 18% of all cases(1,2). Most affected patients require surgery to restore the function of the extensor apparatus(3). Only in cases of partial rupture involving less than 50% of the tendon and with preservation of active extension may conservative management be considered in the form of immobilization of the knee in extension during a period of two weeks(4).
Patellar tendon injury can occur at three levels: at its proximal insertion in the lower pole of the patella; in the body of the tendon; or at its distal insertion in the anterior tuberosity of the tibia. The options for the surgical management of tendon body rupture include end-to-end suturing, either isolatedly or in combination with other techniques such as cerclage, ischiotibial autografting or allografts(5). The choice depends on the time of rupture and the degree of degeneration.
With regard to the time elapsed from rupture, and although there is no consensus on the definition of chronicity(4), some articles describe a period of two weeks as the limit for considering a lesion to be acute, as in the study published by Gilmore et al., in a review of 503 patellar tendon ruptures. In their study, lesions classified as chronic presented an important failure rate of 14-20% with simple repair techniques, though the percentage was seen to decrease on combining augmentation procedures (cerclage and autografts)(5).
The literature describes different augmentation techniques, though there is no clear agreement as to which option is best. Synthetic meshes for augmentation have been used in the repair of other tendons such as the quadriceps tendon, with good results. Their use in repair of the patellar tendon is therefore also considered(6). We present a case of chronic rupture of the patellar tendon that was subjected to end-to-end suturing with augmentation using a synthetic polyethylene terephthalate mesh.
Material and methods
Clinical case
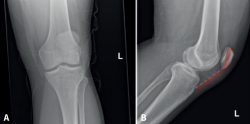
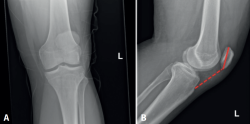
A 44-year-old male with no relevant disease history presented due to persistent functional impotency of the left knee following direct low-energy trauma to the joint three weeks ago. Exploration evidenced swelling of the pre-patellar region, with impossibility of extending the knee against gravity, and with the axe-stroke sign in the middle third of the patellar tendon. The anteroposterior and lateral radiographs of the knee evidenced a high patella (Figure 1).
Chronic rupture of the middle third of the patellar tendon was diagnosed, and surgery was decided for repair of the tendon using end-to-end suturing with synthetic polyethylene terephthalate mesh (Trevira®) augmentation, based on the technique described below.
Surgical technique
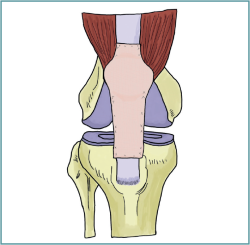
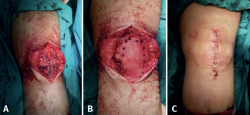
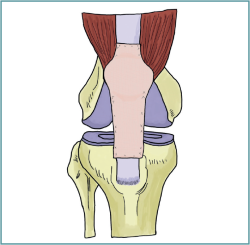
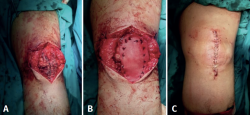
With the patient in the supine position and placing the ischemia cuff on the affected limb, an anterior approach was used centered on the patellar tendon from the proximal pole of the patella to the anterior tibial tuberosity. The lesion was identified, evidencing degeneration and retraction of both tendon margins. Debridement of the lesion was performed in a first step. End-to-end suturing was then performed using the double Krackow technique on both ends of the tendon, employing non-reabsorbable, braided high-resistance suture (Ethibond®) composed of polyethylene and with reinforcing stitches in the peritenon. Subsequently, in view of the poor quality of the tendon tissue, the synthetic mesh was placed and sutured over the tendon for augmentation of the tendon repair, using non-reabsorbable sutures (Figure 2). It should be mentioned that such suturing was made with the leg extended, in order to maintain a degree of tension in the mesh on flexing the knee. Finally, the subcutaneous tissue was closed with reabsorbable sutures, and the skin with staples (Figure 3).
Following surgery, the knee was immobilized in full extension with orthosis for three weeks. Isometric quadriceps exercises were started in the immediate postoperative period. Weight bearing with two crutches was allowed after two weeks, with the orthosis blocked in extension. After three weeks the patient was allowed to progressively start flexion-extension exercises of the knee, increasing flexion by 30º every week with the aim of securing complete motion range after 8 weeks. Partial weight bearing without orthosis was authorized after 8 weeks, with full weight bearing after 12 weeks. At follow-up after 6 months, the patient presented full range of motion of the knee (Figure 4), with a pain score on the visual analogue scale of 0 and a Knee Society Score (KSS) of 92. Knee function was seen to be preserved with respect to that of the contralateral limb.
Discussion
In acute rupture where end-to-end suturing is not possible, in chronic rupture, in recurrent rupture and in greatly degenerated tendons, it seems necessary to use techniques additional to end-to-end suturing, since the latter alone is insufficient because of the deficient quality of the remaining tendon tissue, thus complicating the healing process(3,7).
Thus, the use of primary repair augmentation systems may improve the stability of repair and the healing rate in cases characterized by prolonged evolution and important tendon degeneration(8). Schliemann et al. carried out a biomechanical study in cadavers, involving the different patellar tendon repair techniques. These authors concluded that there is a significant difference in terms of repair stability with the use of augmentation techniques (suture or cable cerclage), and recommended their use for preventing loss of reduction of the repair, and for allowing greater safety in early mobilization(9).
Although no large series of patients with chronic patellar tendon injuries have been published, autografting currently appears to be the best available method, since it has been associated with a lesser failure rate than other methods such as cerclage or sutures associated to primary repair(5). Chen et al. described two cases of augmentation with semitendinosus tendon and gracilis muscle autografts, with good results(10). Mafulli et al. in turn published a series of 19 cases of patellar tendon repair using ischiotibial grafts, with good functional recovery in all patients. Nevertheless, they described possible complications of the technique, such as intraoperative fracture of the patella or of the anterior tibial tuberosity(11). The use of quadriceps tendon autografts has also been reported, and patellar tendon from the contralateral side has even been employed(4).
Likewise, allografts can be employed, though their biological potential is more limited, with added immune and disease transmissibility problems that cause their use to be limited to cases characterized by great tendon tissue loss, with the aim of reconstructing the ligament (not augmentation)(12). For example, Iacono et al. described the reconstruction of chronic patellar tendon rupture after failed primary repair in a patient with Ehlers-Danlos syndrome, proposing the use of allografts in cases with systemic collagen fiber involvement(13).
Studies involving the use of synthetic ligaments have also been published. Harato et al.(1) described a case in which artificial ligament was used as a patellar tendon substitute in a patient with chronic rupture, though they reported technical difficulty in maintaining correct tension of the structure. Following the operation, flexion was progressively limited to 120º after three months, with definitive suspension of immobilization after one year. The more longer outcomes with the use of this technique are not known. Likewise, Naim et al. described another case in which artificial ligament was applied in a patient with chronic patellar tendon damage, with good mobility results after one year of follow-up(14).
The Trevira® reconstruction mesh is principally composed of polyethylene terephthalate, conforming a structure containing 200 µm pores and with a tensile strength of 4000 N. Its cost is about 600 euros. It is primarily used in megaprostheses for tendon and muscle anchoring, since it allows broader and more stable contact between the soft tissue and the prosthesis. It induces a minimal immune response and affords very good integration, since the mesh provides an adequate scaffold for tissue growth in the patient(15). In this sense, the development of connective tissue in the mesh has been described, with no appearance of granulomas or inflammatory phenomena in the anchoring zone(16). Furthermore, the synthetic mesh affords a substrate for immediate suture fixation, since the patient tissue is often friable and affected(17).
The use of synthetic meshes as a tendon repair method has increased in recent years. Abdel et al. used a synthetic mesh for repair in 77 patients with chronic lesions of the extensor apparatus following total knee arthroplasty, with good results in 84% of the cases. However, 12 patients, of which 5 presented patellar tendon rupture, required revision of the synthetic mesh due to failure of the latter(18). The literature also describes a case in which it has been used as augmentation strategy in chronic rupture of the quadriceps tendon after primary repair failure, being seen as an alternative in native tendon(19).
The main advantage of using this mesh versus autologous grafting is that it poses less patient morbidity, since complications have been reported at the autograft donor site. One problem is pain at the donor site; although considered to be temporary in most patients, such pain may prove persistent in some cases. As an example, Correy et al. reported a donor site pain rate of 6% two years after the operation(20). Another important problem is the obtainment of an insufficient ischiotibial graft length due to its early amputation at harvesting, which may make it necessary to obtain another graft(21). Other complications have also been described, such as damage to the saphenous nerve and to the medial collateral ligament(22). In relation to the reconstruction technique, patella fracture may occur on performing the intraosseous tunnels(11). Gregory et al. described three cases in which patellar fracture occurred after tunnel preparation in patients subjected to extensor apparatus repair surgery(23). On the other hand, the synthetic mesh allows anchoring of the patellar tendon to the quadriceps tendon, affording greater stability, while in the case of autografting this depends on its extent. However, it must be noted that synthetic meshes imply very high costs and possess a lesser biological potential than autografts.
Conclusions
A range of options are available for patellar tendon rupture repair. A case is described in which a synthetic polyethylene mesh was used as a complement to primary repair of chronic patellar tendon rupture, demonstrating its viability and satisfactory functional outcomes.