Arthroscopic core decompression of the femoral head with autologous stem cell placement as treatment for femoral head osteonecrosis
Descompresión central de la cabeza femoral artroscópica más colocación de células madre autólogas como tratamiento de la osteonecrosis de la cabeza femoral
Resumen:
La osteonecrosis de la cabeza femoral (ONCF) es una patología multifactorial, incapacitante, causada por la interrupción, la disminución o el daño del aporte sanguíneo de la cabeza femoral de manera constante y repetitiva. El manejo de esta patología está dirigido a abordar de forma sinérgica los factores de riesgo, el diagnóstico temprano y la preservación articular. La descompresión central (DC) del fémur es actualmente el procedimiento recomendado en estadios tempranos antes del colapso de la cabeza femoral y tiene como objetivo mejorar el aporte sanguíneo, disminuir la presión intraósea y estimular la neovascularización. La DC puede realizarse mediante abordaje lateral y artroscópico, teniendo como ventaja este último el abordaje concomitante de otras patologías intraarticulares (95% lesiones asociadas) y extraarticulares de la cadera con menores tasas de complicaciones. La técnica artroscópica permite localizar el sitio de necrosis en la cabeza femoral con mayor precisión durante la DC, reduce el riesgo de lesión cartilaginosa, disminuye la morbilidad y el riesgo de fracturas. La DC se puede acompañar de la implantación de células madre en la zona de necrosis con resultados favorables. El objetivo de este artículo es describir la técnica quirúrgica artroscópica de DC artroscópica más colocación de células madre. La técnica consiste en realizar un abordaje artroscópico de cadera mediante 3 portales con técnica dentro fuera. Se realiza el tratamiento de patologías concomitantes (pincer, reparación labral y cam). Posteriormente, se localiza la zona de necrosis avascular mediante escopia y se verifica la ausencia de ausencia de colapso mediante artroscopia. Bajo visión directa se realizan 6 perforaciones de 1,3 mm y 3 perforaciones de 2,8 mm con separación de 3 mm. Tras ello se comprueba el sangrado. Finalmente, se retira la solución de irrigación y se colocan las células madre autólogas previamente cosechadas a través de una perforación de 2,8 mm y bajo control por escopia.
Nivel de evidencia: IV.
Abstract:
Osteonecrosis of the femoral head (ONFH) is a multifactorial disabling condition produced by constant and repetitive disruption, reduction or damage to the blood supply of the femoral head. Its management seeks to synergically address the risk factors, ensure an early diagnosis, and preserve the affected joint. Arthroscopic core decompression (CD) of the femur is currently recommended in the early stages, before collapse of the femoral head, and aims to improve the blood supply, reduce intraosseous pressure, and stimulate neovascularization. Core decompression can be performed via a lateral and arthroscopic approach, with the advantage of being able to concomitantly address other intraarticular disorders (95% of associated lesions) and extraarticular alterations of the hip, with fewer complications. The arthroscopic technique allows us to locate the site of femoral head necrosis with greater precision during CD, reduce the risk of cartilage damage, and lessen morbidity and the risk of fractures. In turn, CD may be accompanied by stem cell placement in the necrotic zone, with favourable results. The present study describes the arthroscopic CD with stem cell placement technique. The latter involves an arthroscopic approach to the hip using three portals with an inside-out technique. Treatment of the concomitant disorders is carried out (pincer, labral repair and cam). Then, the necrotic zone is located visually, with arthroscopic verification of the absence of collapse. Under direct vision, 6 perforations measuring 1.3 mm and three perforations measuring 2.8 mm are made, with a separation of 3 mm. Following this, bleeding is checked. Lastly, the irrigation solution is withdrawn and the previously harvested stem cells are placed through a 2.8 mm perforation under visual control.
Level of evidence: IV.
Introduction
Osteonecrosis of the femoral head (ONFH) is a multifactorial disabling condition produced by constant and repetitive disruption, reduction or damage to the subchondral blood supply. It causes cell death and the accumulation of microfractures, with subsequent non-maintained bone remodeling and the generation of changes in bone architecture, producing joint pain and functional disability(1,2). Overall, ONFH is responsible for 5-12% of all hip joint replacement surgeries(2,3).
The main objective of treatment is to synergically address the risk factors and bone necrosis in the early phases. However, in up to 95% of all patients, associated deformities have been identified in the form of cam lesions (82%), labral defects (85%) or chondral defects (74%). These disorders can be managed through hip arthroscopy(4). The reported advantages of this minimally invasive procedure are greater precision during core decompression (CD), reduction of the risk of joint cartilage damage, and lesser morbidity and fracture risk(5,6,7).
Thus, arthroscopic decompression eliminates the risks inherent to open surgery, with a decrease in complications, less postoperative pain and a shorter recovery time(5).
The present study describes the arthroscopic CD technique associated with stem cell placement and the management of concomitant lesions.
Clinical case
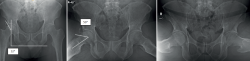
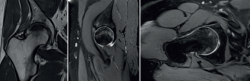
A 45-year-old male presented with no relevant medical history. He reported due to right hip pain with no known cause. The pain worsened with physical activity, the standing position, and prolonged sitting. Exploration evidenced painful flexion 120º, painful abduction 40º, adduction 30º, painful internal rotation 15º and painful external rotation 25º. Maneuvers: FABER (flexion, abduction and external rotation) test +, FADIR (flexion, adduction and internal rotation) test + and log roll +; medical functional Hip Outcome Score (HOS) 35/68 points (51.5%), and pain visual analogue scale 7/10. The anteroposterior and 90º Dunn position radiographic study of the pelvis evidenced femoral head sclerosis, in addition to cam and pincer type morphology (Figure 1). Magnetic resonance imaging of the right hip showed a hypointense image in T2-weighted sequencing, with hyperintense margins in T1-weighted sequencing (double contour sign), acetabular labrum tearing corresponding to Czerny-Hoffman(8) grade IIIA, thinning of the joint cartilage and no collapse of the femoral head. the Kerboul angle(9) was 284°, with a high risk of collapse of the femoral head (Figure 2).
Mixed femoroacetabular impingement syndrome was diagnosed, associated with a Czerny-Hoffman grade IIIA labral lesion plus avascular necrosis of the femoral head corresponding to ARCO(10) stage IIc. Since this was a young and active adult with no additional comorbidities, joint preservation treatment was decided with hip arthroscopy. The imaging studies showed no evidence of degenerative alterations or collapse of the femoral head(11,12).
reacae.30380.fs2304012en-figure2.png

Figure 2. Magnetic resonance imaging of the right hip showing a hypointense image in T2-weighted sequencing in the coronal and axial views, with hyperintense margins in T1-weighted sequencing (double contour sign), pincer and cam lesion, acetabular labrum tearing corresponding to Czerny-Hoffman grade IIIA, and thinning of the joint cartilage. Measurement of the Kerboul angle corresponding to 284°.
Surgical technique
Stem cell harvesting, placement and portals
Surgery was performed by an experienced surgeon (CNS). With the patient in supine decubitus and under combined (spinal and general) anesthesia, with aseptic and antiseptic measures, bone marrow aspiration was performed to obtain autologous mesenchymal stem cells from the left iliac crest using the T-LokTM Bone Marrow Biopsy Needle 11 Gaus × 4 Inches (Argon Medical Devices Inc., TX, USA).
The patient was placed on the orthopedic traction table in supine decubitus, with protection of the genital area and lower extremities. The hip to be operated upon was placed in adduction 5º, flexion 15º and internal rotation 15º. After skin marking of the anatomical references, traction was applied, limited to the minimum needed to achieve opening of the joint space to about 10 mm. The standard arthroscopic portals for the procedure were prepared (anterolateral, middle anterior and accessory distal anterolateral) for visioning and operation with the inside-out technique(13,14).
Arthroscopy, pincer resection, labral repair and cam resection
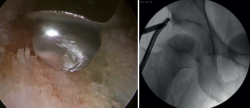
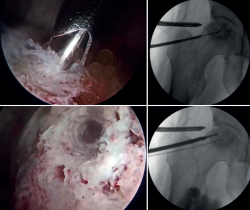
An interportal linear capsulotomy was performed to access the coxofemoral joint. Then, acetabuloplasty was carried out with the over the top technique for resection of the pincer lesion(Figure 3).
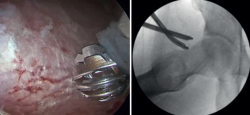
Repair of the labral lesion was made with two knotless PEEK anchors measuring 2.8 mm (PopLok® Knotless Suture Anchor, ConMed Corp., New York, USA) and a 1.3 mm knotted anchor (Y-Knot® Flex, ConMed Corp., New York, USA). Microperforations were made in the grade II acetabular chondral lesion, measuring 1.0 × 1.0 cm2 (Figure 4).
Traction was then suspended and the cam lesion was resected (Figure 5).
Arthroscopic core decompression
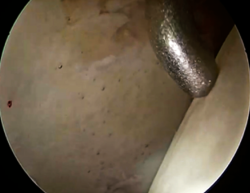
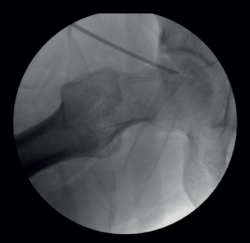
After treatment of the concomitant disorders, the femoral head lesion was visually identified and the absence of femoral head collapse at the site of necrosis was checked arthroscopically (Figure 6).
Six perforations were made with the guide of the 1.3 mm anchors (Y-Knot® Flex) and three perforations were made with the guide of the 2.8 mm knotless PEEK anchors (PopLok® Knotless Suture Anchor) for CD of the femoral head through the anterolateral region of the femoral neck under visual guidance, establishing a separation of 3 mm between them, with a diameter of 1.3 mm and 2.8 mm, respectively, and checking bleeding of each perforation (Figure 7 and Video 1).
Placement of the autologous stem cells
Aspiration of the irrigation solution was performed. By means of a perforation made with the guide of the 2.8 mm knotless PEEK anchors (PopLok® Knotless Suture Anchor), measuring 2.8 mm in diameter, the previously harvested autologous stem cells were placed under visual control. Lastly, capsule closure was carried out using high resistance sutures, with sealing of the portals. The total duration of surgery was three hours and 15 minutes; one hour and 30 minutes with traction of the lower extremity (Figure 8).
Postoperative management
The patient was discharged on the following day with analgesic medication and no nonsteroidal antiinflammatory drug use. Instructions were provided to avoid weight bearing of the extremity during four weeks, with passive mobilization exercises to gradually gain range of motion.
One month after surgery the patient presented a HOS score of 46/85 points (67.6%) and a pain VAS score of 3/10. Progressive partial weight bearing was started, with active complete ranges of motion, muscle strengthening, walking retraining and gradual discontinuation of supports.
At follow-up four months after surgery, the patient presented HOS score of 61/68 points (89.7%) and a pain VAS score of 0/10. The imaging studies showed a decrease in the zone of necrosis of the femoral head, with improvement of the Kerboul angle from 284° to 240° (Figures 9 and 10). In relation to complications, the patient presented heterotopic ossification with an image measuring 0.8 mm in diameter at extraarticular level proximal to the femoral neck.
Six months after surgery, the physical examination revealed full ranges of mobility, with no pain, and negative joint impingement maneuvers.
Discussion
Core decompression is the gold standard for the treatment of ONFH. Traditionally, CD has been performed using a retrograde and percutaneous protocol through a lateral approach to the femur in the subtrochanteric region(2). Many authors such as Mont(15) in 2004 and Song(16) in 2007 introduced the concept of percutaneous decompression with multiple orifices through the femoral neck, using a lateral approach under imaging guidance. In turn, in 2006, Yan et al. introduced CD with the use of growth factors and cell differentiation factors, with promising results(17).
A systematic review published in 2017 reported superior outcomes with the use of cell therapy in ONFH versus the control group, evidencing a disease progression rate of 24.5% versus 40%, respectively, and a total hip replacement conversion rate of 16% versus 21% in the control group(2).
The experts recommend multiple perforations in order to maximize the efficacy of the procedure(18).
A systematic review was carried out by Hua in 2019, comprising 32 studies with 2441 hips: 1379 subjected to isolated CD, 565 treated with CD combined with autologous bone, and 497 subjected to CD combined with bone marrow. The success rate in the first group was 57%, versus 74% in the CD plus bone marrow group, and 81% in the last group. The clinical results evidence a general success rate with the three procedures of 65%, with statistically significant differences between them. The conclusion was that CD is an effective and safe method for the treatment of ONFH. This procedure, associated to the placement of autologous bone and bone marrow, increases the success rate, and caution is advised in cases of advanced stages(19).
Another systematic review was carried out by Liu in 2021, with the inclusion of 784 patients (918 hips), and involving the evaluation of 7 different surgeries: isolated CD, CD with bone grafting, CD with tantalum implantation, CD with cell therapy, CD with bone grafting and cell therapy, vascularized bone graft, and conservative management. In relation to the radiological progression findings, CD and cell therapy afforded better results, followed by isolated CD. It thus was concluded to be a possible option for delaying progression of the disease based on the current evidence(20).
Core decompression of the femoral head with the implantation of mesenchymal stem cells from bone marrow was first described in 2002 by Hernigou(21). A study carried out in 2015 by Persiani, involving 31 hips with ONFH treated with CD plus the implantation of mesenchymal stem cells from bone marrow, recorded improvement of the symptoms and the resolution of osteonecrosis in stages I and II in 25 hips. In addition, progression to osteoarthritis was observed in 6 hips (2 stage II, 2 stage III and 2 stage IV). It was concluded that joint pain decreased, as evaluated with the Harris Hip Score (HHS), VAS and 12-item short-form survey (SF-12). Likewise, the procedure was considered to be successful, avoiding or delaying the need for joint replacement surgery in the early stages of ONFH, as evaluated from radiographs and magnetic resonance imaging studies(22).
Another study published in 2018 reported that the use of stem cells as treatment for ONFH is efficient and safe in patients with ARCO stages I and II(23). Lastly, a systematic review of randomized controlled trials published in 2020, with the inclusion of 13 randomized clinical trials (855 hips), reported that the use of stem cells in ONFH delays collapse of the femoral head (relative risk: 0.54) and the need for hip replacement surgery (relative risk: 0.55), with a statistically significant difference in relation to adverse effects(24).
The adaptation of decompression performed via the arthroscopic route eliminates the risks inherent to open surgery, reduces the number of complications, lessens postoperative pain, and shortens the time to recovery(5).
A study carried out in 2023 by Ji included 185 hips with ONFH in ARCO stages I (n=43), II (n=114) and III (n=28), subjected to joint debridement and multiple small bone perforations via arthroscopy. The survival rates were 79%, 72%, 52%, 32% and 10% in patients in stages I, IIa, IIb, IIc and III, respectively. The authors concluded that CD is effective in patients with ONFH in its early stages, particularly in those with associated joint hip disease conditions(25).
The results obtained with the technique described in this study are similar to those found in the international literature. No objective comparisons can be established, however, due to the short follow-up period involved and the fact that this is a case report and a description of the surgical technique. The patient showed clear functional improvement, with an important decrease in pain, avoiding collapse of the femoral head, and with no major complications. Thus, CD of the femoral head plus the placement of autologous stem cells as treatment for ONFH via arthroscopy is a viable therapeutic alternative.
A limitation of this study is the short follow-up time involved. Although the study was not intended to report on results, it does describe a reproducible surgical technique. Furthermore, it presents the case of the treated patient and the control imaging findings that evidence a decrease in Kerboul angle despite the short postsurgical time, with improvement from high to moderate risk of collapse. Two factors may explain the clinical improvement. Firstly, concomitant disease conditions were treated in the same procedure (femoroacetabular impingement and labral repair), and secondly, although the imaging studies after four months did not evidence complete resolution of the necrosis, the appearance of neovascularization and the formation of new trabecular bone made it possible to avoid collapse of the femoral head.
Conclusions
Arthroscopic CD with the placement of autologous stem cells as treatment for ONFH affords favorable results over the short term, as evidenced both in the literature and in the present study, making it possible to treat associated disorders with few complications compared with non-arthroscopic decompression. The technique thus should be considered as an option in patients with ONFH.
Supplementary material
The video of the technique accompanying this article can be seen at (Video 1):
Figuras
Figure 1. Anteroposterior (AP) radiographic view of the pelvis and 90º Dunn position study showing an increased center-edge angle of Wiberg of 50º and an increased alpha angle of 60º.
Figure 2. Magnetic resonance imaging of the right hip showing a hypointense image in T2-weighted sequencing in the coronal and axial views, with hyperintense margins in T1-weighted sequencing (double contour sign), pincer and cam lesion, acetabular labrum tearing corresponding to Czerny-Hoffman grade IIIA, and thinning of the joint cartilage. Measurement of the Kerboul angle corresponding to 284°.
Figure 3. Arthroscopic acetabuloplasty using the over-the-top technique. Control of the procedure with image intensifier.
Figure 4. Labral repair with anchorings, affording adequate stabilization checked through palpation and performing microperforations in the chondral lesion.
Figure 7. Core decompression of the femur through microperforations; arthroscopic view and fluoroscopic control.
Figure 9. Anteroposterior (AP) radiographic view of the pelvis and 45º and 90º Dunn position, four months after surgery.
Información del artículo
Cita bibliográfica
Autores
Carlos Navarrete Sarasty
Hospital Metropolitano. Quito, Ecuador
Byron Torres Dávila
Hospital Metropolitano. Quito, Ecuador
Pablo Cueva González
Hospital Metropolitano. Quito, Ecuador
Carlos Peñaherrera Carrillo
Hospital Metropolitano. Quito, Ecuador
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Hua KC, Yang XG, Feng JT, et al. The efficacy and safety of core decompression for the treatment of femoral head necrosis: a systematic review and meta-analysis. J Orthop Surg Res. 2019;14(1):306.
-
2Piuzzi NS, Chahla J, Schrock JB, et al. Evidence for the use of cell-based therapy for the treatment of osteonecrosis of the femoral head: a systematic review of the literature. J Arthroplasty. 2017;32(5):1698-708.
-
3Mont MA, Carbone JJ, Fairbank AC. Core decompression versus nonoperative management for osteonecrosis of the hip. Clin Orthop Relat Res. 1996;324(324):169-78.
-
4Serong S, Haubold J, Theysohn J, Landgraeber S. Arthroscopic assessment of concomitant intraarticular pathologies in patients with osteonecrosis of the femoral head. J Hip Preserv Surg. 2020;7(3):458-65.
-
5Day HK, Shelton TJ, Comfort SM, et al. Arthroscopic core decompression for avascular necrosis of the femoral head using multiple small-diameter tunnels. Arthrosc Tech. 2022;11(11):e1879-82.
-
6Theopold J, Armonies S, Pieroh P, Hepp P, Roth A. Nontraumatic avascular necrosis of the femoral head: Arthroscopic and navigation-supported core decompression. Oper Orthop Traumatol. 2020;32:107-15.
-
7Nazal MR, Parsa A, Martin SD. Mid-term outcomes of arthroscopic-assisted Core decompression of Precollapse osteonecrosis of femoral head-minimum of 5 year follow-up. BMC Musculoskelet Disord. 2019 Oct 15;20(1):448.
-
8Czerny C, Hofmann S, Neuhold A, et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology. 1996;200(1):225-30.
-
9Takashima K, Sakai T, Hamada H, Takao M, Sugano N. Which classification system is most useful for classifying osteonecrosis of the femoral head? Clin Orthop Relat Res. 2018;476(6):1240-9.
-
10Yoon BH, Mont MA, Koo KH, et al. The 2019 revised version of Association Research Circulation Osseous staging system of osteonecrosis of the femoral head. J Arthroplasty. 2020;35(4):933-40.
-
11Marín-Peña O, Lund B, Ayeni OR, Dantas P, Griffin D, Khanduja V. Basic Concepts in Hip Arthroscopy. In: ESSKA Instructional Course Lecture Book. Berlín, Heidelberg: Springer; 2018. pp. 45-67.
-
12Byrd T. Indications and Contraindications. En: Operative Hip Arthroscopy. Springer; 2006. pp. 6-35.
-
13Sandoval E, Cimas D. Técnicas de posicionamiento y abordaje en artroscopia de cadera. Portales. Rev Esp Artrosc Cir Articul. 2016;23(1):31-6.
-
14Pérez-Carro L, Galindo C, Estany E, Adrio RG, Golano P, Vega J. Hip Arthroscopy Indications and Technique. Roma: CIC Edicione Internationale Tecnique Chirurgiche in Ortopedia e Traumatologia Hip Arthroscopy Indications and Technique; 2011. pp. 9-16.
-
15Etienne G, Mont MA, Ragland PS. The diagnosis and treatment of nontraumatic osteonecrosis of the femoral head. Instr Course Lect. 2004;53.
-
16Song WS, Yoo JJ, Kim YM, Kim HJ. Results of multiple drilling compared with those of conventional methods of core decompression. Clin Orthop Relat Res. 2007;454:139-46.
-
17Marker DR, Seyler TM, Ulrich SD, Srivastava S, Mont MA. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res. 2008;466(5):1093-103.
-
18Microsurgery Department of the Orthopedics Branch of the Chinese Medical Doctor Association, Group from the Osteonecrosis and Bone Defect Branch of the Chinese Association of Reparative and Reconstructive Surgery, Microsurgery and Reconstructive Surgery Group of the Orthopedics Branch of the Chinese Medical Association. Chinese guideline for the diagnosis and treatment of osteonecrosis of the femoral head in adults: Guideline for ONFH. Orthop Surg. 2017;9(1):3-12.
-
19Hua KC, Yang XG, Feng JT, et al. The efficacy and safety of core decompression for the treatment of femoral head necrosis: a systematic review and meta-analysis. J Orthop Surg Res. 2019;14(1):306.
-
20Liu Q, Guo W, Li R, Lee JH. Efficacy of various core decompression techniques versus non-operative treatment for osteonecrosis of the femoral head: a systemic review and network meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. 2021;22(1):948.
-
21Hernigou P, Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002;405(405):14-23.
-
22Persiani P, De Cristo C, Graci J, Noia G, Gurzì M, Villani C. Stage-related results in treatment of hip osteonecrosis with core-decompression and autologous mesenchymal stem cells. Acta Orthop Belg. 2015;81(3):406-12.
-
23Li R, Lin QX, Liang XZ, et al. Stem cell therapy for treating osteonecrosis of the femoral head: From clinical applications to related basic research. Stem Cell Res Ther. 2018;9(1).
-
24Mao L, Jiang P, Lei X, et al. Efficacy and safety of stem cell therapy for the early-stage osteonecrosis of femoral head: a systematic review and meta-analysis of randomized controlled trials. Stem Cell Res Ther. 2020;11(1).
-
25Ji Q, Li X, Luo S, et al. Long-term outcomes of arthroscopic synovectomy and core decompression through multiple small bone holes for early-stage avascular necrosis of the femoral head. Arthroplasty. 2023;5(1):17.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- From the start to the top: the history of knee osteotomies
- Clinical-functional and radiographic outcomes of medial valgus-producing tibial osteotomy
- Patellar tendinopathy: a practical consensus guide for choosing the best treatment
- Evolution of spinal endoscopy. Where do we come from and where are we going?
- Partial ruptures of the rotator cuff
- Arthroscopic core decompression of the femoral head with autologous stem cell placement as treatment for femoral head osteonecrosis
- Extraarticular plasty as sole maneuver in the correction of rotational instability due to rupture of the anterior cruciate ligament in an elderly patient
- Fully arthroscopic osteosynthesis with button placement in acute anterior glenoid fracture: a case report
- Arthroscopic visualization of the popliteal hiatus and localization of an intraarticular free body
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.