Direct reattachment in anterior cruciate ligament ruptures
Reinserción directa en roturas del ligamento cruzado anterior
Resumen:
El enfoque terapéutico de las roturas del ligamento cruzado anterior (LCA) ha evolucionado en los últimos 50 años. La publicación de malos resultados con la técnica de reparación directa (popularizada en los años setenta) motivó su abandono en favor de técnicas de reconstrucción con plastias, aunque el interés por la reinserción del LCA se ha reavivado recientemente por el desarrollo de nuevas técnicas quirúrgicas y la mejora del instrumental y los implantes empleados en ellas.
Las ventajas de la reparación directa frente a la reconstrucción incluyen la ausencia de morbilidad en la zona donante, una menor agresividad quirúrgica, la preservación del tejido nativo, un aparente menor tiempo de recuperación y la facilidad para realizar una cirugía de revisión en caso de rerrotura. Las técnicas de reinserción podrían estar indicadas en el caso de roturas proximales del ligamento (tipos 1 o 2 de la clasificación de Sherman) con buena calidad de tejido, siempre y cuando se trate de cirugía en agudo o con poco tiempo de evolución sobre adultos de mayor edad que no practiquen deportes de contacto.
En esta publicación se describen la técnica de reinserción directa al fémur con un implante sin nudos y la técnica de suspensión cortical. En ambos casos, la reparación se acompaña de un refuerzo sintético, pudiendo valorarse además la asociación de un refuerzo extraarticular anterolateral.
La técnica de sutura directa se está popularizando y puede ser una herramienta más en la cirugía de las lesiones del LCA. Si bien los resultados son esperanzadores, todavía no están bien definidas las indicaciones en cuanto a la cronología y el grado de actividad, la edad y la demanda deportiva de los pacientes. Son necesarios ensayos clínicos bien diseñados, incluyendo el tratamiento conservador, que ayuden en la toma de decisiones. Es fundamental seleccionar adecuadamente la rotura y el paciente para obtener el mejor resultado posible.
Abstract:
The therapeutic approach to anterior cruciate ligament (ACL) tears has evolved over the past 50 years. The publication of poor results with the direct repair technique (popularized in the 1970s) led to its abandonment in favour of plasty reconstruction techniques, although interest in ACL reattachment has recently been rekindled by the development of new surgical techniques and improved instruments and implants.
The advantages of direct repair over reconstruction include the absence of donor site morbidity, less surgical aggressiveness, preservation of native tissue, an apparently shorter recovery time, and the ease of performing revision surgery in case of re-rupture. Reattachment techniques may be indicated in the case of proximal ligament ruptures (types 1 or 2 of the Shermanclassification) with good tissue quality, provided that surgery is performed in the acute or short term in older adults who do not play contact sports.
The present study describes the direct femoral reattachment technique with a knotless implant and the cortical suspension technique. In both cases, repair is accompanied by synthetic reinforcement, and the addition of anterolateral extra-articular reinforcement may also be considered.
The direct suture technique is gaining popularity, and may be an additional tool in the surgery of ACL injuries. While the results are encouraging, the indications are not yet well established in terms of chronology and activity level, patient age and sporting demands. Well-designed clinical trials, including conservative treatment, are needed to help in decision-making. Proper selection of the tear and of the patient is essential to secure the best possible result.
Introduction
The therapeutic approach to anterior cruciate ligament (ACL) tears has evolved over the last 50 years and, as is often the case in our speciality, some techniques that had been abandoned due to poor results are revived with improved materials and instruments. In the case of ACL surgery, we are witnessing a growing interest in direct ACL repair as an alternative to reconstructive surgery.
In the 1970s, the technique described by Feagin(1) involving direct reattachment of the ACL via arthrotomy followed by prolonged immobilization, became popular. The treatment of meniscal disorders and other associated injuries was obviously not the same as it is today. The initial results were good, but mid-term review evidenced disappointing outcomes, with a high incidence of pain (71%) and residual instability (94%)(2). These poor results led to the abandonment of direct reattachment in favor of plasty reconstruction techniques.
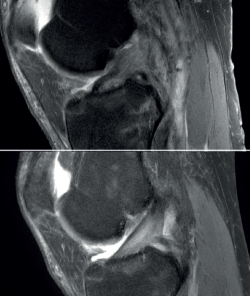
We now know from the histological study of ACL remnants after rupture that the ligament has some intrinsic capacity for spontaneous healing, as evidenced by the presence of vascular buds, nerve endings and cells with healing capacity in the remnant tissue(3). Further evidence of this self-repairing capacity can be found in the good functional results published in some patients treated on a conservative basis, especially older individuals with lesser physical demands(4) (Figure 1).
Despite this, it is true that complete healing of the ACL without surgical treatment after rupture is rare. Among other reasons, this is because of the presence of synovial fluid inside the joint, which hinders the formation of a contained hematoma between the two extremities of the torn ligament (a necessary preliminary step for tissue healing). To overcome this adverse joint environment and improve the results of ACL reconstruction, a number of authors(5) have for some years recommended preserving the remains of the torn ligament, taking advantage of its biological capacity to facilitate its integration into the bone tunnels and improve proprioception.
The present study describes two techniques for ACL repair that maximize the idea of preserving the remnant tissue, taking full advantage of its healing potential in order to heal it in its femoral footprint.
Indications
The advantages of direct repair over ligament reconstruction include the absence of donor site morbidity, reduced surgical aggressiveness, the preservation of native tissue, a shorter recovery time, and a reduced complexity of eventual revision surgery in case of failure(6).
The main indication for primary ACL repair is in patients with high-grade complete or partial tears corresponding to types 1 or 2 of the original Shermanclassification(7), i.e. in avulsions of the femoral insertion (type 1) or in proximal tears leaving 75-90% of the distal ligament intact (type 2). In any case, good quality of the remaining tissue is essential. It should be noted that the incidence of tears of this kind appears to be greater in individuals over 35 years of age(7). This is not a problem, given that the incidence of re-rupture following ACL repair is higher in younger patients under 21 years of age(8,9).
With regard to the timing of surgery, the operation is ideally performed within 6 weeks of the injury(10,11,12), although good results have also been published repairing chronic tears in which the torn ACL stump heals over the posterior cruciate ligament (PCL)(13,14).
It is also important to add that the results of ACL repair seem to be improved by combining other techniques, such as reinforcement with a synthetic suture tape (InternalBrace®), which has shown better biomechanical results in studies on cadavers(11), or anterolateral reinforcement procedures (extra-articular tenodesis, anterolateral ligament repair)(15,16).
Direct femoral fixation technique
Instruments
The technique requires two closed loop sutures(FiberLink® from Arthrex, Naples, FL, USA;UltraLoop® from Smith & Nephew, Andover, MA, USA), a suture passer(Scorpion® from Arthrex; FirstPassMini® from Smith & Nephew), two threaded 4.75 mm knotless implants with their respective punches(SwiveLock® 4.75 mm from Arthrex,HealiCoil® from Smith & Nephew), a tape(FiberTape® from Arthrex,UltraTape® from Smith & Nephew), and a 2.4 mm drill. The procedure should be performed by a surgeon experienced in knee arthroscopy.
Surgical technique
The patient is placed in the supine position and the leg is draped and prepared for knee arthroscopy at the surgeon's discretion, as if an ACL plasty were to be performed. The anterolateral and anteromedial portals are established as usual, and the joint is explored. On exploring the central compartment, it should be confirmed by direct vision and also palpation that the lesion is proximal and that the tissue quality is good; if the tissue is friable and tears easily, repair is not indicated. If the ACL remnant is attached to the PCL, it must be dissected so that the ACL is free and can be manipulated to its insertion site. A blunt shoulder arthroscopy periosteotome is best used for this, although a synoviotome, vaporizer or plasma applicator could also be used, as long as care is taken not to break or burn the tissue and render it non-viable. If there are concomitant meniscal or cartilage lesions, they should be treated earlier in order to avoid forced varus and valgus positions after the repair is completed.
After having confirmed the proximal lesion of the ACL and the good quality of the remnant ligament tissue, and having treated any accompanying injuries in the other compartments, an accessory anteromedial portal is prepared. It is important to widely resect Hoffa's fat pad to improve vision, facilitate passage of the threads, and prevent the latter from adhering to soft tissues. A cannula, ideally flexible (PassPort® from Arthrex), should be used to prevent the threads from adhering to the soft tissues, although this is not essential. The use of long cannulas, such as shoulder cannulas, is not ideal, as they extend too far outside the skin and greatly restrict use of the instruments.
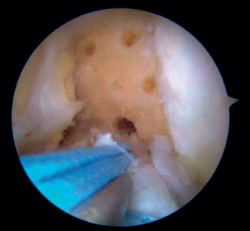
Once a good view of the central compartment is obtained, the area of the femoral footprint of the ACL is prepared to leave exposed bone, and microperforations are made in the medial wall of the lateral condyle to leave a bleeding bed to favor healing of the ligament (Figure 3). These microperforations can be made using specific instruments or with the implant punch. The advantage of using the punch is that the implant insertion site can be prepared at the same time, and only one instrument is used for the entire process (Figure 4). This step can be done after the suture has been prepared in the ligament, although doing it beforehand avoids the threads from standing in the way. The ideal point for fixation is just anterior to the native ACL footprint, although if the tear is partial or corresponds to Sherman I, it can be taken to the anatomical footprint without difficulty.
The anteromedial and posterolateral fascicles of the ACL are then identified for suturing separately. Using a suture passer, a closed loop suture is passed through the anteromedial fascicle at its most distal zone, and the loopless extremity is carried alternately (medial to lateral, lateral to medial and so on) to the most proximal zone, usually involving 3 or 4 passes of the suture. The thread may knot on itself during suturing if we are not attentive to it on entry and exit. To solve this problem, we simply undo the knot with retrieval forceps and repeat the step if necessary.
On completion, the thread is retrieved through the accessory anteromedial portal. The process is then repeated, this time with the posterolateral fascicle. To prevent the first thread from breaking with passage of the second thread, it must be ensured that entry and exit in the ligament are very posterior and ideally somewhat proximal to those used for the anteromedial fascicle. Once having reached the most proximal zone after 3 or 4 passes, retrieval is carried out in the same way through the accessory anteromedial portal.
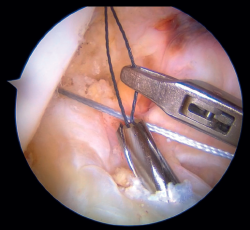
Outside the knee, the threads are loaded into a knotless anchor implant with a tape that will act as anterior reinforcement of the ACL when attached to the tibia. Once the implant has been loaded, it is inserted into the previously prepared site. This step is facilitated when viewing is made from the anteromedial portal, as it affords a better perspective of the zone (Figure 5). Once the implant has been inserted, the suture threads are cut at the level of the condylar wall.
With vision through the anterolateral portal, the tibial guide of the ACL is placed in the central zone of its distal insertion, and a tunnel is made with a 2.4 mm cannulated drill through which a loop-ended nitinol is passed and retrieved through the accessory anteromedial portal. The nitinol serves as a retriever, to load the tape through it and pass it through the tibial tunnel. Once the tape is retrieved, it is secured to the tibial cortex with a knotless anchor implant or button, tightening the tape with the knee in near full extension. If a threaded implant is used, it is important to check that no implant threads protrude at the cortex, as this could cause discomfort in the future.
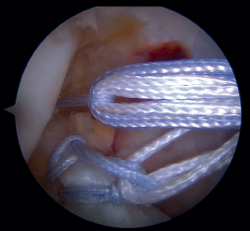
Under arthroscopic vision, it is important to confirm tension of the ACL both in the full range of motion and with the use of a palpator and the Lachman and anterior drawer maneuvers (Figure 6).
Cortical suspension technique
Instruments
This technique requires a short arthroscopy cannula (PassPort®, Arthrex), femoral and tibial drill guides for the ACL, 4.5 mm and 2.4 mm drills, two retriever sutures (EthiBondLoop® #5, Johnson & Johnson, NJ, USA), a suture passer (KneeScorpion®, Arthrex; FirstPass Mini, Smith & Nephew), specific sutures (FiberRing®, Arthrex), a cortical suspension system(ACL RepairTightRope®, Arthrex), a biotenodesis implant (SwiveLock® 4.75 mm, Arthrex; HealiCoil, Smith & Nephew), and the instruments needed to perform bone marrow stimulation techniques. As an alternative to the Arthrex cortical suspension device, we can use the LigaBrace® system from Smith & Nephew, which involves some technical differences with respect to the procedure described below.
Surgical technique
The patient can be placed in the position each surgeon prefers for ACL reconstruction surgery. As with the direct fixation technique, this procedure begins by using the usual anterior portals in knee arthroscopy: a high, anterolateral portal and a standard anteromedial portal. Similarly, the ACL is examined with a palpator to confirm the tear and its suitability for repair.
The next step consists of introducing the necessary instruments through the anteromedial portal to make several perforations approximately 1 mm deep in the femoral insertional footprint, with the aforementioned aim of obtaining a bleeding bed to facilitate healing of the ACL. Such drilling can be done manually (with micro- or nanofracture punches) or motorized (PowerPick®, Arthrex), and this step is usually made easier by flexing the knee at about 100°.
Once the bone marrow is stimulated, a short silicone cannula (PassPort®) is placed in the anteromedial portal with the help of vascular forceps. This cannula will help us to organize the suture threads and will make it difficult for Hoffa's fat pad and other soft tissues to get in the way. With the same aim of facilitating suture management (and drilling of the femoral tunnel), an accessory medial portal is now added, in a position medial to the anteromedial portal.
The femoral tunnel is made from this accessory medial portal using a 4.5 mm diameter spear point drill, from the most anterior portion of the insertional footprint of the ACL through the lateral cortex of the femur. Once the tunnel has been completed, the same drill is used to leave a retriever thread through the femoral tunnel, as it is equipped with an eyelet. It is important to secure the two ends of this thread together outside of the knee in order to avoid losing either of them during surgery.
The tibial tunnel is prepared with a guide inserted through the cannula of the anteromedial portal, passing a 2.4 mm cannulated drill from the medial cortex of the tibia to the most anterior region of the tibial footprint of the ACL, taking care to damage the ligament fibers as little as possible during this step.
Once the tunnel has been drilled, the guide is removed from the inside of the drill and another retriever thread is inserted through it. This thread is extracted using grasping forceps inserted through the cannula from the anteromedial portal to outside the knee (Figure 7), where it is likewise secured, as was already done with the femoral retriever thread.
Then, and also through the cannula, arthroscopic suture forceps (KneeScorpion®, FirstPass® Mini) loaded with an ultra-high strength suture specific for this technique (FiberRing®) is introduced. Using the forceps, the suture thread is passed through the distal third of the stump of the ACL, with both ends exiting through the cannula after removal of the instrument from the joint. After removing this first thread, the steps are repeated in identical fashion with a second suture, which now passes through the ligament in a more proximal position. It is very important that these two sutures pass completely through the full thickness of the ACL.
Our attention now turns to outside the knee, where the loop of the cortical suspension system (ACL Repair TightRope®) is secured to the ACL using the FiberRing® sutures. This device is a cortical suspension button with a loop of variable length, which also incorporates a high strength tape. To secure it, the suture marked as "1" on the card is first passed through the retriever thread of one of the FiberRing® sutures, and then the step is repeated through the retriever thread of the remaining FiberRing® suture. Next, this thread passing through the rings of the FiberRing® system is passed through the closed loop marked as "2". Finally, this thread is passed through the nitinol marked "3"; the card is held firmly and the nitinol is pulled so that the TightRope® thread passes through the cortical plate. At this point, part of the loop, the button and the threads connected to it (loop traction sutures, button lift sutures and high strength tape) remain outside the knee, waiting to be inserted into the joint (Figure 8).
The next step is to remove the femoral retriever thread through the cannula of the anteromedial portal, loading it with the traction and flipping sutures, but not with the high strength tape. By pulling on the retriever thread, the ACL RepairTightRope® sutures will pass through the femoral tunnel (Figure 9), exiting through the skin. Using the lift sutures, the button is then likewise advanced through the tunnel until it is flipped over the lateral femoral cortex (which can be checked by pulling firmly on the high strength tape, which still exits through the cannula). At this point, all that remains is to pull alternately on both loop traction sutures to shorten the loop and reduce the stump of the ACL until contact is made with its native footprint.
As the last step of the procedure, the high strength tape connected to the cortical button is retrieved through the anteromedial portal, where the tibial tunnel retriever thread is located. By loading the tape onto the thread and pulling on it, the tape now lies in front of the repaired ligament and exits through the anteromedial cortex of the tibia, where it is fixed with the knee fully extended with a tenodesis implant (SwiveLock®, HealiCoil®). After completing the procedure, it is advisable to check the tension of the ligament and the InternalBrace®, as well as the absence of impingements and limitations in mobility of the knee (Figure 10).
Postoperative management
Both free mobility and immediate support with an articulated orthosis locked in extension for weight bearing is allowed, unless there is some concomitant injury preventing full support or early mobilization(17) - although not all authors suggest the use of the orthosis(18). From the outset, the patient can perform isometric quadriceps exercises and mobility exercises to regain full range of motion. If used, the orthosis can be gradually removed once the protective function of the quadriceps is restored. Progressive impact exercises are allowed from three months, and unrestricted activities (including sports activities) are allowed once full neuromuscular control is achieved, approximately 4-6 months after surgery(19).
Discussion
The direct suture technique is gaining popularity, and may be an additional tool in the surgery of ACL injuries. At present, this treatment option is indicated for proximal ACL tears (types 1 and 2 of the Shermanclassification)(7), with good quality remnant tissue, and performed ideally within the first 6 weeks after injury. Some aspects that are still not entirely clear are, precisely, the surgical window of opportunity (some authors have published good results repairing chronic ruptures)(13,14), patient age (at present, caution is advised on indicating the procedure in younger patients, due to their greater risk of failure)(8,9), and the level of activity of the patient.
It is true that the results published to date are encouraging, but it is no less true that most of the publications are from working groups with a special interest in this technique (involving small samples and shortfollow-up periods)(17), and have not necessarily been widely reproduced(20,21). More studies are needed on the results and re-rupture rates between standard reconstruction and direct suturing, but also compared to conservative treatment groups, in order to be able to generalize this technique.
While it may be a surgically less aggressive technique, the systematic combination of anterolateral extra-articular tenodesis with direct repair, as proposed by some authors, may make the surgery less conservative(15,16). The justification that in the event of failure, revision surgery is simpler (comparing more to primary reconstruction rather than revision surgery), should not make us forget that the patient has already undergone a lengthy surgery and postoperative period.
The ACL possesses healing capacity. The fundamental problem may be the formation of a space between the proximal stump and the wall of the lateral condyle in the insertion footprint. This space, occupied by synovial fluid, may inhibit the formation of an organized hematoma and proper healing of the ligament. The problem may be more mechanical than biological(3). The development of specific techniques such as those described above can improve this situation (Figure 11), but does not guarantee healing or the absence of a separating gap between the extremities that would hinder healing(22).
The possibility of repairing an ACL tear depends on the characteristics of the tear itself and of the patient. With regard to the tear, according to the Sherman classification , 22% of all ACL tears are considered to correspond to type 1 (avulsions of the femoral insertion), 90% of which present sufficient tissue quality to indicate repair(23).
The likelihood of a good outcome following ACL repair decreases as the time between injury and surgery increases, due to progressive deterioration of the histology of the remnant(24). Fortunately, however, it is not necessary to wait for the knee to regain full mobility after ligament rupture before repair can be carried out.
Although according to some studies, early surgical treatment is associated with an increased risk of postoperative stiffness following ACL reconstruction(25), this is not a concern when using repair techniques, as in fact, patients undergoing ACL repair have a greater range of motion in the immediate postoperative period than those undergoing ligament reconstruction, since the surgery is less aggressive and avoids the drilling of large diameter tunnels and the morbidity associated with autograft harvesting. The only factor that has been associated with a decrease in postoperative range of motion is the repair of associated meniscal lesions (as also occurs with reconstructions), whereas, interestingly, the presence of chondral lesions does not appear to affect the range of motion(6).
In addition to the characteristics of the lesion, mention also must be made of characteristics referred to the patient: younger and more active patients may have a higher risk of re-rupture after direct repair(20). Proper selection of the tear and of the patient is essential to secure the best possible result.
Conclusions
Direct ACL repair techniques are becoming popular despite the fact that the indications are not clearly established, given the absence of well-designed clinical trials that include conservative management and help in decision making(26). Direct reattachment is a safe technique and can be a less surgically aggressive option, with shorter recovery times and good results in older, non-high demand patients with proximal Sherman type 1 tears and good tissue quality, treated on an acute basis, combining the use of an InternalBrace® and assessing the need to add an anterolateral extra-articular reinforcement technique.
The surgeon's attitude towards innovations in our speciality requires an open mind, but also a critical view. Generalization of the use of these techniques should be based on comparative studies with proven reconstruction techniques.
Supplementary material
The video of the technique accompanying this article can be seen at (Video 1):
Figuras
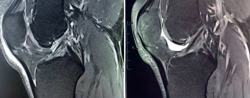
Figure 1. Tearing of the anterior cruciate ligament (ACL). A: sagittal magnetic resonance imaging (MRI) view of an acute tear at diagnosis; B: MRI control after 12 months with conservative treatment, showing evident improvement in the image of the ligament.
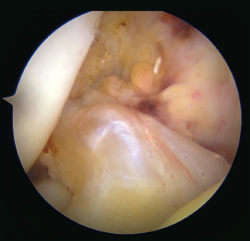
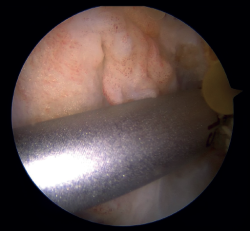
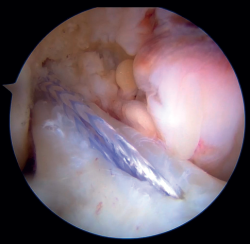
Figure 2. Image of a Sherman type 1 anterior cruciate ligament (ACL) tear with good tissue quality. Right knee, view from the anterolateral portal.
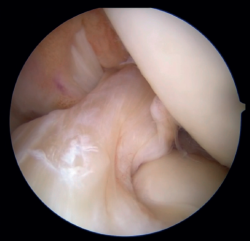
Figure 3. Microperforations in the medial wall of the external femoral condyle, adjacent to the insertion of the anterior cruciate ligament (ACL), to stimulate reattachment healing. Left knee, view from the anteromedial portal.
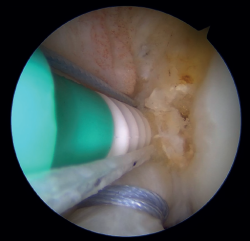
Figure 4. Punch perforation of the medial wall of the external femoral condyle for subsequent knotless implant placement in the femoral fixation with implant technique. Left knee, view from the anterolateral portal.
Figure 5. Suture fixation of the external femoral condyle using a knotless implant (SwiveLock®, Arthrex). Left knee, view from the anterolateral portal.
Figure 6. Final view of the repair after placement of the InternalBrace® with high strength tape. Left knee, view from the anterolateral portal.
Figure 7. Tibial tunneling with a 2.4 mm cannulated drill for nitinol passing and placement of the InternalBrace® with high strength tape. Right knee, view from the anterolateral portal.
Figure 8. Insertion of the cortical fixation system including the high strength tape for InternalBrace® reinforcement. Right knee.
Figure 9. Passing of the cortical fixation system after joining with the sutures passed through the anterior cruciate ligament (ACL). Right knee, view from the anterolateral portal.
Figure 10. Final result of direct anterior cruciate ligament (ACL) repair with the cortical fixation system and InternalBrace® with high strength tape. Right knee, view from the anterolateral portal.
Figure 11. Pre- (image at left) and postoperative appearance (image at right) of an anterior cruciate ligament (ACL) tear subjected to direct repair.
Información del artículo
Cita bibliográfica
Autores
Diego García-Germán Vázquez
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario HM Torrelodones. Universidad San Pablo CEU. Torrelodones. Madrid
Clínica DKF. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Central de la Cruz Roja San José y Santa Adela. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Puerta de Hierro-Majadahonda. Majadahonda. Madrid
Javier Ruiz Diaz
Ibermutua. Oviedo
Hospital Ibermutua Asturias
Jaime Dalla Rosa Nogales
Hospital Quirónsalud Málaga
Hospital Vithas Parque San Antonio. Málaga
Complejo Hospitalario Integral Privado (CHIP). Málaga
Agencia Sanitaria Costa del Sol. Marbella, Málaga
Pablo Crespo Hernández
Sección de Miembro Inferior. Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Ramón y Cajal, Madrid
Editor invitado
Hospital Universitario HM-Sanchinarro. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that the procedures carried out abided with the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Feagin JA, Curl WW. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med. 1976;4(3):95-100.
-
2Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I. The long-term followup of primary anterior cruciate ligament repair. Defining a rationale for augmentation. Am J Sports Med. 1991;19(3):243-55.
-
3Nguyen DT, Ramwadhdoebe TH, van der Hart CP, Blankevoort L, Tak PP, van Dijk CN. Intrinsic healing response of the human anterior cruciate ligament: An histological study of reattached ACL remnants. J Orthop Res. 2014;32(2): 296-301.
-
4Hetsroni I, Delos D, Fives G, Boyle BW, Lillemoe K, Marx RG. Nonoperative treatment for anterior cruciate ligament injury in recreational alpine skiers. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1910-4.
-
5Van Keulen LZ, Hoogeslag RAG, Brouwer RW, Huis In't Veld R, Verdonschot N. The importance of continuous remnant preservation in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2022;30(5):1818-27.
-
6Van Der List JP, DiFelice GS. Range of motion and complications following primary repair versus reconstruction of the anterior cruciate ligament. Knee. 2017;24(4):798-807.
-
7Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I. The long-term followup of primary anterior cruciate ligament repair. Defining a rationale for augmentation. Am J Sports Med. 1991;19(3):243-55.
-
8Vermeijden HD, Yang XA, van der List JP, DiFelice GS. Role of age on success of arthroscopic primary repair of proximal anterior cruciate ligament tears. Arthroscopy. 2021;37(4):1194-201.
-
9Rilk S, Goodhart GC, van der List JP, et al. Anterior cruciate ligament primary repair revision rates are increased in skeletally mature patients under the age of 21 compared to reconstruction, while adults (>21 years) show no significant difference: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2024. Epub ahead of print.
-
10Douoguih WA, Apseloff NA, Murray JC, Kelly RL, Svoboda SJ. Suture-augmented anterior cruciate ligament repair for proximal avulsion or high-grade partial tears shows similar side-to-side difference and no clinical differences at two years versus conventional anterior cruciate ligament reconstruction for mid-substance tears or poor anterior cruciate ligament tissue quality. Arthroscopy. 2024;40(3):857-67.
-
11Wilson WT, Hopper GP, Banger MS, Blyth MJG, Riches PE, MacKay GM. Anterior cruciate ligament repair with internal brace augmentation: a systematic review. Knee. 2022;35:192-200.
-
12Douoguih WA, Zade RT, Bodendorfer BM, Siddiqui Y, Lincoln AE. Anterior cruciate ligament repair with suture augmentation for proximal avulsion injuries. Arthrosc Sports Med Rehabil. 2020;2(5):e475-e480.
-
13Van der List JP, DiFelice GS. Preservation of the anterior cruciate ligament: a treatment algorithm based on tear location and tissue quality. Am J Orthop (Belle Mead NJ). 2016;45(7):e393-e405.
-
14Rilk S, Vermeijden HD, van der List JP, DiFelice GS. Anterior cruciate ligament primary repair is a valid treatment option for proximal tears with good to excellent tissue quality in the acute, sub-acute and delayed setting - A letter to the editor. J ISAKOS. 2024;9(4):740-1.
-
15Deviendri R, van der Veen HC. Isolated lateral extra-articular tenodesis enhance better rotatory knee joint stability post-primary ACL repair: four cases report and literature review. Int J Surg Case Rep. 2021;84:106167.
-
16Ferretti A, Carrozzo A, Saithna A, et al. Comparison of primary repair of the anterior cruciate ligament and anterolateral structures to reconstruction and lateral extra-articular tenodesis at 2-year follow-up. Am J Sports Med. 2023;51(9):2300-12.
-
17Jonkergouw A, van der List JP, DiFelice GS. Arthroscopic primary repair of proximal anterior cruciate ligament tears: outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):21-8.
-
18Wu J, Kator JL, Zarro M, Leong NL. Rehabilitation principles to consider for anterior cruciate ligament repair. Sports Health. 2022;14(3):424-32.
-
19Heusdens CHW, Hopper GP, Dossche L, Roelant E, Mackay GM. Anterior cruciate ligament repair with Independent Suture Tape Reinforcement: a case series with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):60-7.
-
20Gagliardi AG, Carry PM, Parikh HB, Traver JL, Howell DR, Albright JC. ACL repair with suture ligament augmentation is associated with a high failure rate among adolescent patients. Am J Sports Med. 2019;47(3): 560-6.
-
21Osti M, El Attal R, Doskar W, Höck P, Smekal V. High complication rate following dynamic intraligamentary stabilization for primary repair of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):29-36.
-
22Bachmaier S, DiFelice GS, Sonnery-Cottet B, et al. Treatment of acute proximal anterior cruciate ligament tears—Part 2. The role of internal bracing on gap formation and stabilization of repair techniques. Orthop J Sports Med. 2020;8(1):2325967119897423.
-
23Van der List JP, DiFelice GS. Preoperative magnetic resonance imaging predicts eligibility for arthroscopic primary anterior cruciate ligament repair. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):660-71.
-
24Margarian AM, Fleming BC, Harrison SL, Mastrangelo AN, Badger GJ, Murray MM. Delay of 2 or 6 weeks adversely affects the functional outcome of augmented primary repair of the porcine anterior cruciate ligament Am J Sports Med. 2010;38(12):2528-34.
-
25Hopper H, Adsit M, Reiter CR, et al. Female sex, older age, earlier surgery, anticoagulant use, and meniscal repair are associated with increased risk of manipulation under anesthesia or lysis of adhesions for arthrofibrosis after anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2024;40(5):1687-99.
-
26Engebretsen L. Editorial commentary: The anterior cruciate ligament cannot be reliably repaired: studies with a control group are needed! Arthroscopy. 2020;36(2):613-4.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Learning from the best
- Everyone's effort
- Inclusion of the long portion of the biceps in rotator cuff repairs
- Surgical technique of the arthroscopic Latarjet procedure with button fixation
- Arthroscopic lateral collateral ligament plication of the elbow
- Arthroscopy-assisted treatment of metacarpophalangeal joint fractures of the fingers
- Surgical technique of hip arthroscopy without perineal post
- Direct reattachment in anterior cruciate ligament ruptures
- Application of fresh osteochondral allografts to the patella. Surgical procedure
- Arthroscopic ligamentoplasty for lateral ankle instability
- Two handles to grasp: double bucket-handle meniscal lesion
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.