Arthroscopic lateral collateral ligament plication of the elbow
Plicatura artroscópica del ligamento colateral lateral del codo
Resumen:
La posterolateral rotatoria del codo es la inestabilidad más frecuente que encontramos en dicha articulación, causando dolor en la cara lateral y limitación funcional en los pacientes que la padecen. El gold standard es la reconstrucción ligamentosa del complejo lateral, pero en las inestabilidades que se presentan como subluxaciones de la cabeza radial o luxaciones de esta sin incluir la articulación ulnohumeral una plicatura artroscópica del ligamento puede ser la solución al problema con menor disección de las partes blandas y menor tiempo de rehabilitación.
El objetivo de este artículo es describir dicha técnica artroscópica como solución a este tipo de inestabilidad.
Abstract:
Posterolateral rotator cuff instability is the most common instability found in the elbow joint, causing pain on the lateral aspect and functional limitation in patients who suffer from this condition. The gold standard is ligamentous reconstruction of the lateral complex. However, in instabilities such as radial head subluxations or radial head dislocations not involving the ulnohumeral joint, arthroscopic ligament plication may be the solution to the problem, with less soft tissue dissection and less rehabilitation time.
The present article describes this arthroscopic technique as a solution for this type of instability.
Introduction
Posterolateral rotatory instability of the elbow was described by O'Driscoll et al.(1) in 1991. It is the most common chronic instability of the elbow(2), and is generally a consequence of trauma, although it can also be seen in the context of recurrent corticosteroid infiltrations or following surgery for epicondylar pain.
Patients often complain of pain in the lateral aspect of the elbow with occasional popping and the inability to perform pushing movements such as rising from a chair or doing push-ups.
The usual treatment is open reconstruction of the lateral collateral ligament complex of the elbow (LCL) using allografts or autografts(2,3,4).
Although this technique has excellent success rates(5) in terms of stabilization, it requires extensive soft tissue dissection and prolonged rehabilitation periods.
With the development of elbow arthroscopy, other forms of diagnosis(6) and treatment began to be considered and, in 2019, Dr. Roger van Riet described arthroscopic plication of the lateral complex(7) based on a previous technique by Dr. Smith in 2001(8), with presentation of the first short-term clinical outcomes in 2022(9).
The aim of the technique is to secure re-tensioning of the posterolateral structures of the elbow (capsule, ligament and anconeus) to eliminate joint instability in cases of grade 1 and 2 posterolateral instabilities in which the quality of the tissue is insufficient for re-anchoring, but there is sufficient tissue to allow plication.
The present article provides a technical description of arthroscopic plication according to Dr. van Riet.
Surgical technique
Expectations
This technique is a minimally invasive alternative to the gold standard technique, involving a shorter surgery time and good postoperative stability rates, along with shortened rehabilitation periods(9).
Indications
Grade 1 posterolateral rotatory instability of the elbow(10): this is the most benign presentation of posterolateral instability, in which there is subluxation of the radial head with elbow extension and supination, the patients showing positive signs of instability such as pivot shift or chair rise.
Grade 2 posterolateral rotatory instability of the elbow(10): this is the intermediate stage presentation, with complete or near-complete dislocation of the radial head at extension and supination with varus instability.
Contraindications
- Persistent acute instability of the elbow in which ligament re-anchoring is possible.
- Grade 3 posterolateral rotatory instability of the elbow(10): this is the most severe presentation, with associated ulnohumeral dislocations, which will require graft-based reconstruction.
Instruments
- Basic arthroscopy equipment for the elbow (shoulder equipment may be used).
- Synoviotome.
- 14G needle or Abbocath through which a PDS 2 suture can be passed.
- Three PDS 2 sutures (non-braided resorbable monofilament).
- Straight mosquito or grasping forceps.
Description of the technique
The patient is positioned in lateral decubitus, with the arm to be operated upon hanging free and supported in such a way as to allow greater than90° flexion of the elbow, which should be located approximately at the level of the surgeon's waist. Care should be taken to protect the bony prominences of the knees, and it is advisable to place a rolled sheet under the armpit in contact with the stretcher to protect the plexus. The healthy arm is positioned on a support adjacent to the patient's face, ensuring that it does not interfere with the surgical field.
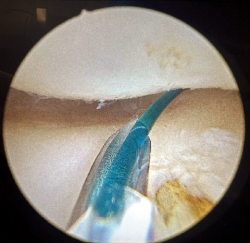
After cleaning, sterile draping and before the ischemia increase, the portals to be used and the trajectory of the lateral elbow complex are painted on the skin. We mark the following: epicondyle and epitrochlea, tip of the olecranon and radial head.
We likewise mark the usual direct central posterior, posterolateral and soft spot portals, as well as the anterior portals. Finally, we mark the trajectory (origin and insertion) of the lateral elbow complex with a line from the center of the epicondyle to the supinator crest, which we mark slightly radial to the subcutaneous border of the ulna at the level of the radial neck (Figure 1).
The technique is performed entirely in the posterolateral compartment of the elbow, where the origin of the lateral complex is located. Anterior compartment arthroscopy may be performed previously in order to confirm the diagnosis of instability on observing an increase in radiocapitellar distance with varus stress of the forearm.
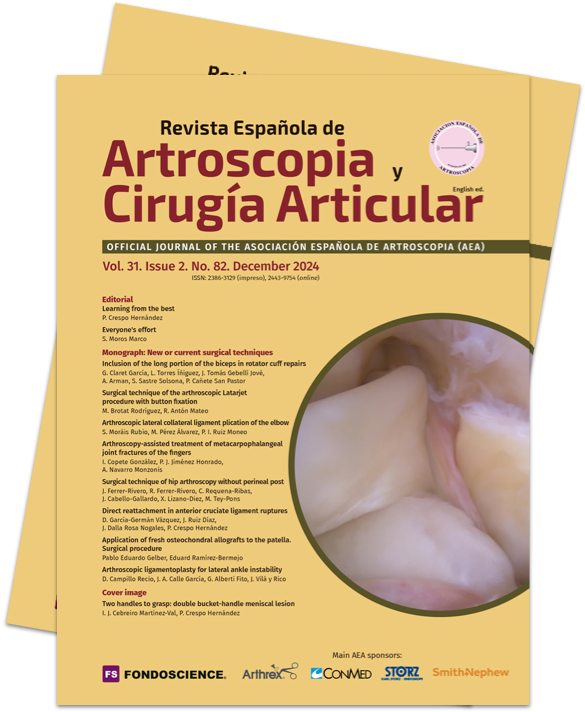
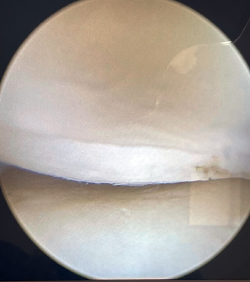
Visioning for lateral complex plication is made through the posterolateral portal. From this portal we access the lateral elbow groove to visualize the posterior part of the radiocapitellar joint. It will also allow us to examine the Osborne-Cotterill lesion component and determine the degree of posterolateral instability by applying varus and supination to the forearm. With this maneuver we can observe how the radial head undergoes subluxation posteriorly and the joint line opens (Figure 2).
To perform the plication we will need a 14G needle or an Abbocath through which a PDS 2 suture or some other type of non-braided resorbable suture can pass, together with three of these sutures.
Observing the lateral groove from the posterolateral portal, we introduce an Abbocath with a PDS type suture from the origin of the LCL at the center of the epicondyle in an intra-articular direction to the lateral groove. Recovery of the suture is made using grasping or straight mosquito forceps at the level of the soft spot.
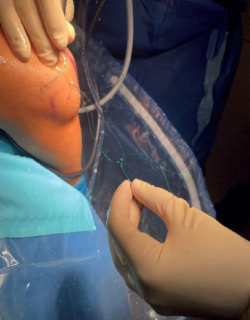
The same Abbocath with another PDS type suture is introduced through the skin at the level of the LCL insertion at the supinator crest along the subcutaneous border of the ulna towards the lateral groove. It is important to stay close to the bone with the needle deep to the anconeus, in order to avoid nerve injury and to include it in the plication (Figure 3).
Once the needle is positioned intra-articular, the suture is recovered again through the same soft spot.
At this point we will have two sutures exiting through the soft spot; we will knot them together (Figure 4) to recover them by pulling on the suture located at the origin of the LCL. In this way we will have a single intra-articular suture extending from the insertion to the origin of the LCL, exiting through the skin in both places (Figure 5).
Another suture of the same type is taken folded in half and transported intra-articular using the previous suture, so that, by making a cut at the looped end, we have two suture strands at both skin exit points (Figure 6).
Using a straight mosquito, one end of the suture is retrieved subcutaneously at the soft spot from the origin of the LCL, and the other end is retrieved from the insertion of the LCL (Figure 7).
The subcutaneous pass is then made again with the other piece of suture.
If tension is now applied to both sutures and we observe from the posterolateral portal, the radiocapitellar joint is seen to close following plication (Figure 8).
The arthroscope is removed from the joint, and the two ends are sutured separately, taking care to bury the knots as deep as possible at subcutaneous level.
These sutures now plicate the lateral elbow complex, the capsule and part of the anconeus, by grasping from the intra-articular epicondyle to the supinator crest and exiting through the anconeus to the subcutaneous tissue back to the epicondyle. Inclusion of the anconeus in the capsule-ligament plication procedure allows the maximum amount of biological tissue to be included in the plication, thus giving it greater consistency.
reacae.31282.fs2312032en-figure9.png

Figure 9. Schematic drawing of the technique used. From the top left corner to the right. An Abbocath is entered in the lateral epicondyle. It is directed intra-articular to the soft spot and a PDS suture is advanced through it into the joint. The distal end is retrieved at the soft spot. A second suture is inserted into the joint in the same way from the subcutaneous border of the ulna, at the level of the origin of the lateral collateral ligament at the supinator crest. It is retrieved through the soft spot and both sutures are knotted. Traction is applied to one end to leave a single suture running from the lateral epicondyle, intra-articular deep to the lateral capsule to the origin of the lateral complex at the supinator crest and the subcutaneous border of the ulna.
A second suture is folded in half, and the intra-articular suture is used as transport suture. Mosquito forceps are used to retrieve the ends of the sutures at the level of the soft spot for knotting. Illustration courtesy of Dr. van Riet and the MoRe Foundation.
Figure 9 included at the end of the article provides a schematic drawing of the technique (courtesy of Dr. van Riet).
Postsurgical management
The postoperative protocol consists of a hinged elbow brace which the patient can bring for immediate postoperative fitting, or fitting can be made the next day before discharge to limit extension to-60° for the first two weeks,-30° for the next two weeks, and then leave the elbow free. The patient is explained that he/she should avoid ipsilateral shoulder abduction for the first month in order to avoid gravitational varus. The immediate postoperative use of a sling is made for pain relieving reasons and, if the patient feels comfortable, it can be removed.
Muscle strengthening exercises begin at 6 weeks, and unrestricted activity is allowed after three months.
Complications
Subcutaneous knotting is usually the main cause of patient discomfort. However, since PDS is resorbable, this problem usually resolves over time. If the technique is performed using non-resorbable sutures, the knots can be bothersome, but to date the authors have not had to re-operate any patient for this reason.
A possible complication is the limitation of extension if very aggressive plication is performed, although this is a rare situation and does not usually limit the daily life activities of the patient.
On the other hand, consideration is also required of the complications associated with elbow arthroscopy in general, in terms of the possibility of wound infection or neurological damage. However, in this case such situations are quite limited, since the work is done in the posterolateral groove region. Exploration of the anterior compartment is associated with the already known neurological risks.
Rescue procedure
In the case of technical failure (persistence of instability over patient follow-up), formal reconstruction with allograft or autograft would be indicated, based on the traditional techniques.
Discussion
Lateral collateral ligament reconstruction remains the gold standard(1,2,3,4,5) for the treatment of posterolateral elbow instability. However, with the advancement of diagnostic and therapeutic techniques in elbow arthroscopy, alternatives to the above procedure have been sought.
The purpose of the technique described in the present article is to decrease joint instability by tightening the posterolateral structures of the elbow (capsule, ligament and anconeus) in a way similar to the capsular plications performed in patients with shoulder or ankle instability.
Arthroscopic techniques are characterized by a shorter rehabilitation time than reconstructions, avoid donor site morbidity if autografting is used, and involve less soft tissue dissection, which may result in less postoperative pain. However, we are not aware of any current studies comparing the two techniques, which moreover have variations.
Smith(8) was the first to propose arthroscopic plication or imbrication of the lateral complex in 2001, with the intra-articular passing of 1 to 4 resorbable sutures as previously described in this technical note, together with an anchorage at the isometric point of the lateral epicondyle, with another suture to take up all the others in the case of more severe instability - resulting in satisfactory results in more than 20 patients.
Van Riet modified this technique in 2019(7) with the single passing of a double suture, thereby saving surgical time and demonstrating in his 2022 study that at one year, 18 of 19 patients had regained a stable elbow without impairment of joint range of motion. In the mentioned study, 12 patients had grade 1 instability and 6 had grade 2 instability of post-traumatic or post-surgical origin. Eighteen of the patients showed resolution of their signs of instability, and the result was maintained at two years, with improvement of the Mayo Elbow Performance Score (MEPS) from 48 to 88(9). With regard to complications, one patient required ligament reconstruction due to technical failure; one developed stiffness at four months, which was treated through mobilization under anesthesia; and two experienced subcutaneous discomfort related to the suture knotting, which resolved spontaneously.
There are variations of this technique using an anchorage at the isometric point of the lateral epicondyle, such as those proposed by Chanlalit(11) or Arrigoni(12) who after an 18-month follow-up period, recorded stable elbows in four patients, with a return to daily activity without pain and without reporting any complications.
These types of techniques avoid the prominence caused by a subcutaneous suture knot in patients, but imply greater cost and a longer surgery time. To our knowledge, there are no comparative studies between these techniques and the procedure proposed in the present study.
In our case, we performed arthroscopic plication of the lateral collateral ligament of the elbow in 10 patients in the last two years.
In all cases, the signs of instability were resolved, and pain was eliminated in 8 cases.
All but one patient (coincidentally one of the individuals with persistent pain) has returned to work. Nevertheless, follow-up is still short, and these are preliminary results that will need to be confirmed or refuted over long-term follow-up.
The proposed technique is simple and effective in treating grade 1 and 2 rotatory posterolateral instabilities(10). However, it is a recently applied procedure with modifications in which there are still no comparative studies between them or versus the open reconstruction techniques. It therefore remains to be seen over time and with further studies whether it will eventually become the new gold standard.
Figuras
Figure 1. Marking of the arthroscopic portals and planned trajectory of the lateral elbow complex for the plication procedure.
Figure 2. Opening of the radiocapitellar space demonstrating pathological increased laxity of the elbow.
Figure 3. Introduction of one of the intra-articular monofilament sutures, in this case from the insertion of the lateral complex in the ulna.
Figure 6. Final suture transported and cut to obtain two strands. In this case, the technique has been performed with FiberWire®, but some other monofilament or suture can be used according to surgeon preference.
Figure 9. Schematic drawing of the technique used. From the top left corner to the right. An Abbocath is entered in the lateral epicondyle. It is directed intra-articular to the soft spot and a PDS suture is advanced through it into the joint. The distal end is retrieved at the soft spot. A second suture is inserted into the joint in the same way from the subcutaneous border of the ulna, at the level of the origin of the lateral collateral ligament at the supinator crest. It is retrieved through the soft spot and both sutures are knotted. Traction is applied to one end to leave a single suture running from the lateral epicondyle, intra-articular deep to the lateral capsule to the origin of the lateral complex at the supinator crest and the subcutaneous border of the ulna.
A second suture is folded in half, and the intra-articular suture is used as transport suture. Mosquito forceps are used to retrieve the ends of the sutures at the level of the soft spot for knotting. Illustration courtesy of Dr. van Riet and the MoRe Foundation.
Información del artículo
Cita bibliográfica
Autores
Sara Moráis Rubio
Hospital Universitario de Vitoria-Txagorritxu
Mayvet Pérez Álvarez
Hospital Universitario de Vitoria-Txagorritxu
Pedro Ignacio Ruiz Moneo
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Araba
Servicio de Cirugía Ortopédica y Traumatología. Hospital Txagorritxu. Vitoria-Gasteiz
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73:440-6.
-
2Conti M, Caekebeke P, van Riet RP. Lateral collateral ligament injuries of the elbow-chronic posterolateral rotatory instability (PLRI). EFORT Open Rev. 2017;1(12):461-8.
-
3Camp C, Sánchez Sotelo J, Shields M, O’Driscoll S. Lateral Ulnar Collateral Ligament Reconstruction for Posterolateral Rotatory Instability of the Elbow. Arthrosc Tech. 2017;6(4):e1101-e1105.
-
4Sánchez-Sotelo J, Morrey BF, O’Driscoll SW. Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow. J Bone Joint Surg Br. 2005;87-B(1):54-61.
-
5Lin KY, Shen PH, Lee CH, Pan RY, Lin LC, Shen HC. Functional outcomes of surgical reconstruction for posterolateral rotatory instability of the elbow. Injury. 2012;43:1657-61.
-
6Amarasooriya M, Phadnis J. Arthoscopic diagnosis of posterolateral rotatory instability of the elbow. Arthrosc Tech. 2020;9(12):e1951-e1956.
-
7Bain G, Eygendaal D, van Riet RP. Arthroscopic lateral collateral ligament imbrication. Surgical techniques for trauma and sports related injuries of the elbow. New York: Springer; 2019. pp. 263-7.
-
8Smith JP 3rd, Savoie FH 3rd, Field LD. Posterolateral rotatory instability of the elbow. Clin Sports Med. 2001;20:47-58.
-
9Kohlprath R, Vuylsteke K, van Riet RP. Arthroscopic lateral collateral ligament imbrication of the elbow: short-term clinical results. J Shoulder Elbow Surg. 2022;31:2316-21.
-
10O'Driscoll SW, Morrey BF, Korinek S, An KN. Elbow subluxation and dislocation: a spectrum of instability. Clin Orthop Relat Res. 1992;(280):186-97.
-
11Chanlalit C, Mahasupachai N, Sakdapanichkul C. Arthroscopic lateral collateral ligament complex reconstruction for posterolateral rotatory instability of the elbow, the operative technique. Arthrosc Tech. 2021;10(12):e2805-e2812.
-
12Arrigoni P, Ambrosi R, Nicoletti S, Randelli P. Arthroscopic reinsertion of lateral collateral ligament, anterior capsular plication and coronoid tunneling technique for chronic elbow posterolateral rotatory instability. Arthrosc Tech. 2016;5(3):e471-5.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Learning from the best
- Everyone's effort
- Inclusion of the long portion of the biceps in rotator cuff repairs
- Surgical technique of the arthroscopic Latarjet procedure with button fixation
- Arthroscopic lateral collateral ligament plication of the elbow
- Arthroscopy-assisted treatment of metacarpophalangeal joint fractures of the fingers
- Surgical technique of hip arthroscopy without perineal post
- Direct reattachment in anterior cruciate ligament ruptures
- Application of fresh osteochondral allografts to the patella. Surgical procedure
- Arthroscopic ligamentoplasty for lateral ankle instability
- Two handles to grasp: double bucket-handle meniscal lesion
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.