Arthroscopy-assisted treatment of metacarpophalangeal joint fractures of the fingers
Tratamiento asistido por artroscopia de las fracturas de la articulación metacarpofalángica de los dedos
Resumen:
Las indicaciones para la realización de una artroscopia de pequeñas articulaciones de la mano han ido en aumento los últimos años.
Una de las principales indicaciones es la asistencia al tratamiento de fracturas intraarticulares de las articulaciones de los dedos, fundamentalmente la articulación metacarpofalángica. A pesar de ello, todavía es escasa la información que encontramos sobre dicha patología en la bibliografía, pues el número de publicaciones sigue siendo limitado en comparación con el resto de las articulaciones.
En este texto se recogen las pautas y recomendaciones, según nuestra experiencia, para enfrentarse a este tipo de fracturas minimizando la agresión a la articulación y favoreciendo así una mejor y más temprana recuperación funcional.
Abstract:
The indications for arthroscopy of the small joints of the hand have been growing in recent years.
One of the main indications is to assist in the treatment of intra-articular fractures of the finger joints, primarily the metacarpophalangeal joint. Despite this, there is still little information on this disorder in the literature, as the number of publications is still limited compared to the rest of the joints.
This article presents the guidelines and recommendations, based on our experience, for dealing with this type of fracture, minimizing aggression to the joint and thus favoring better and earlier functional recovery.
Introduction
From the beginnings of arthroscopy in the 1960s, the development of different techniques has increased exponentially. In turn, the indications have increased, and this has been reflected in the amount of divulgative material on the topic that is currently available. On the other hand, the parallel development of technology has influenced the use of arthroscopy as an everyday tool for numerous disease conditions. The quality of the optics and the development of instruments have focused attention, along with the ever decreasing size of the instruments. This has contributed to the possibility of arthroscopic interventions targeted to smaller joints.
Arthroscopy of the metacarpophalangeal joint (MCP) was first described by Chen in his article in 1979.
Despite 45 years of history, arthroscopy of small joints is still not a widespread technique today(1). However, technical advances and improvements in our understanding of small joint anatomy have made it possible to evaluate and treat certain disorders amenable to arthroscopic treatment(2,3), including particularly intra-articular fractures, which are the focus of this chapter.
The advantages of small joint arthroscopy over open surgery are numerous and well established. The most important advantages are the reduction of soft tissue damage, which results in a lower risk of post-surgical stiffness(3), and the ability to afford excellent visualization of the articular surface and intra-articular structures(4). However, in order for this benefit to be effective, familiarity with the arthroscopic anatomy of the joint is needed, as well as a learning curve and ideally cadaver practice prior to patient practice.
Presentation of the technique
Surgical anatomy
Although some specific mention should be made when dealing with the thumb, the anatomy of the MCP joint is similar for all fingers. On the dorsal surface of the MCP joint we have the extensor hood, composed of the corresponding extensor tendon and the fibers of the sagittal band that run towards the volar plate. In the case of thumb we have the extensor pollicis brevis (EPB) and the extensor pollicis longus (EPL); and in the second and fifth fingers we find the corresponding extensor tendons. The volar plate is covered by the palmar joint capsule, which is often the site of post-traumatic synovitis(1). Its proximal insertion in the metacarpal is ill-defined, but is clearer along the palmar border of the base of the proximal phalanx. There is often a meniscal rim of the volar plate protruding to the joint space(2).
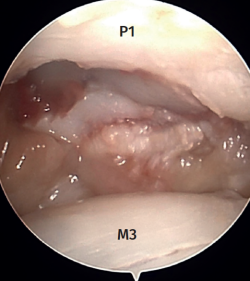
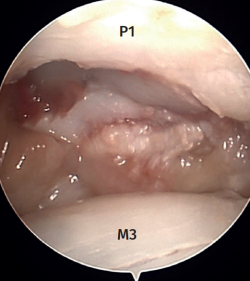
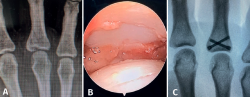
Arthroscopy of the MCP joint allows extensive visualization of the metacarpal head and the base of the proximal phalanx (Figure 1).
In the case of the thumb and sometimes on the radial side of the index finger, we can visualize the sesamoid bones. The radial and ulnar collateral ligaments as well as the accessory ligaments in a more volar position are clearly visible in all the fingers(1). The trajectory of the ligaments can be followed to their origin on both sides of the metacarpal head(2). The insertion of the ligaments at the base of the proximal phalanx is often injured after trauma, and we therefore must be able to identify this.
Thus, the anatomical landmarks to be recognized are, on the one hand, the extensor apparatus, which will serve as a reference for the arthroscopic portals; and, on the other hand, the joint structures themselves, which will be the ones we can visualize during the arthroscopic examination: metacarpal head, base of the proximal phalanx, volar capsule, main and accessory collateral ligaments, and dorsal capsule.
Indications
On reviewing the literature, it should be noted that most publications refer to the MCP joint of the thumb and the trapeziometacarpal joint. Despite this, indications for small joint arthroscopy in general and MCP arthroscopy in particular have progressively been developed and expanded(1,2,4,5,6,7,8), with the most common being the following:
- Inflammatory arthropathy.
- Degenerative osteoarthritis and osteochondral lesions.
- Septic arthritis.
- Removal of free or foreign bodies.
- Collateral ligament injuries.
- Intra-articular fractures.
- Metacarpophalangeal dislocation.
- Joint stiffness.
- Chronic pain.
- Chronic instability.
Below we will focus only on those that are the subject of our work.
Collateral ligament injuries
Ryu and Fargan were the first to describe the arthroscopic management of ulnar collateral ligament injury of the thumb through arthroscopic visualization(6).
Direct visualization of the ligament makes it the most reliable method for assessing the degree of ligament injury and the presence or absence of interposition between the adductor fascia(5).
In terms of treatment, different authors advocate debridement of the insertional area of the ligament, reduction and correct positioning of the bone fragment, and its percutaneous fixation with Kirschner wires(1). Other authors advocate arthroscopy to locate and prepare the ligament and, by means of a minimal incision, re-anchor it(9).
Arthroscopically assisted reduction and percutaneous fixation of the avulsed fragment has several advantages over the open technique(5), including minimal aggression to the joint capsule, which usually serves to shorten the rehabilitation period. Furthermore, although not the subject of our study, the aesthetic result is more pleasing.
Intra-articular fractures
As with Bennett fractures of the thumb, fractures involving the articular surface, both of the common metacarpal head (less commonly) and of the base of the proximal phalanx, can be evaluated and treated with an arthroscopically assisted approach(9).
Kirschner wires can be used both as a method for indirect reduction and as a method for fracture fixation. Alternatively, we can use conventional screws or cannulated screws to fix large fragments. This all depends on the fracture pattern involved, and on the surgeon's expertise and preferences.
There are authors who divide the joint fractures into two groups(1):
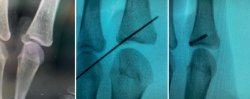
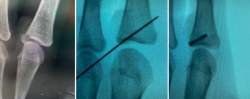
- Fractures with avulsion of the insertion of the collateral ligament (Figures 2 and 3).
- Intra-articular fractures proper, caused by compression or shear mechanisms.
The management of fractures of this kind is the main focus of the present chapter, and the technical details and tips will be presented below.
Contraindications
The contraindications for small joint arthroscopy are similar to those for major joints, including the following(2):
- Poor soft tissue coverage.
- Active cellulite.
- Joint injuries that are obviously beyond the capacity of arthroscopic treatment. In this case the contraindication would be relative, since arthroscopy can be used as a support for the management of these fractures.
The contraindications to the arthroscopic treatment of fractures may be more dependent on the skill or experience of the surgeon(1).
The indications and contraindications for arthroscopy of the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints are similar to those for the MCP joint. There are some particularities in dealing with these joints, but they are beyond the scope of this article.
Instruments and needs
There are different techniques that differ in small details regarding the type of anesthesia used, the force or position in which axial traction is applied, the need for irrigation, the caliber of the optics or instruments, the direction of the portals, or their suture requirements. However, many of these requirements have not been found to be superior to others, or have not been compared.
For this reason, the following is a proposal of our commonly used method for the arthroscopy of small joints, and we also offer a series of tips and tricks based on our experience in the management of fractures of this kind.
As for the material needed, we divide it into two main groups, which are detailed below.
Arthroscopy equipment
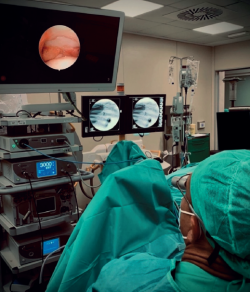
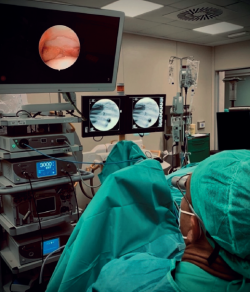
- Arthroscopy tower: Arthrex Synergy UHD4® (Figure 4).
- Arthroscopy traction system: Acumed arc wrist tower.
- Small joint arthroscope (1.9 mm).
- Synoviotome (2.0 mm).
- Traction system with a finger cot or Chinese finger trap.
- Fluoroscopy apparatus.
- Radiofrequency probe (optional).
- Fluid management system (optional).
Specific instruments for fracture management
- Palpator: to assist in fracture reduction from the intra-articular space.
- Kirschner wires of various thicknesses: we use 0.8 wires for fixing smaller fragments, and 1.0 wires for larger fragments and for use as a "joystick" in treating osteochondral fragments. We can also use 1.0 or 1.2 wires to assist fragment mobilization across the fracture site through extra-articular manipulation.
- Freer® blunt elevator (or alternatively a small periostotome).
- Suture anchors.
- Motor.
Technique
The clearest indication is axial compression fractures resulting in central joint collapse, predominantly at the base of the proximal phalanx.
Metacarpal head fractures, although less common, are also amenable to treatment by this method, particularly if comminution is present(1).
Arthroscopy allows removal of any osteochondral fragments, anatomical reduction of the main fragments, synovectomy, and removal of the intra-articular hematoma, as well as (according to some authors), thermal capsular contracture to help reduce the inflammatory process(1).
We advocate the arthroscopic approach to these fractures, not only because it allows more accurate anatomical reduction than can be seen with fluoroscopy, but also because the small aggression involved minimizes the risk of joint fibrosis, which improves recovery time and the functional capacity of the joint.
Patient positioning
Under locoregional anesthesia, the patient is placed in the supine position with the shoulder in abduction and the elbow flexed to 90°.
The affected finger is suspended with the finger trap of a traction device, applying about 3-5 kg.
Some authors advocate performing the procedure under local anesthesia and sedation(1).
The traction force applied per finger was first mentioned in 1999. Since then, articles have been published with ranges of between 2.3 and 5.5 kg (5 to 12 pounds) of traction force(5).
Preparation of the portals
When traction is exerted on the affected finger, depressions are generated on both sides of the extensor apparatus. These will be our references for preparation of the portals. Some authors start by infusing 2-3 ml of saline solution into the joint. In our case, we opt for dry arthroscopy(10).
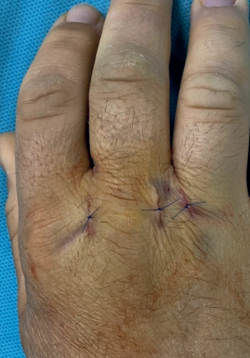
The portals described for MCP arthroscopy are located on both sides of the extensor apparatus: radial and ulnar. At the level of the thumb they should be located radial to the EPB and ulnar to the EPL. A 21G needle is used to locate one of the portals. Then, a longitudinal incision is made with a number 11 scalpel. The longitudinal orientation of the incision, along the axis of movement, promotes healing. Nevertheless, we advocate suturing the portals at the end of the procedure (Figure 5). Incision is made only in the skin in order to avoid iatrogenic damage to the sensory nerves. Then, using a blunt instrument such as straight mosquito forceps, we apply gentle pressure to enter the joint.
reacae.31282.fs2401005en-figure5.png

Figure 5. Location and orientation of the portals on both sides of the extensor apparatus. Although the longitudinal orientation has been the reason why some authors advocate no need for stitches, we advise suturing of the portals at the end of the procedure. In the image, in addition to the portals, we see an accessory incision for the insertion of a cannulated screw.
A blunt trocar is used to introduce the 1.9 mm arthroscope, and joint visualization begins. Generally, 30°optics are used. Using transillumination we locate the contralateral portal (Figure 6) and repeat the process to reproduce the other portal: first we locate with a 21G intramuscular needle, then incise with a scalpel and gently penetrate with mosquito forceps. In doing so, we can alternate the optics and working instruments from one portal to the other, as required. If there is any difficulty in passing the needle into the joint, or if there is any doubt about proper identification of the joint, fluoroscopy can be used to verify the level of the needle before proceeding. As for the synoviotome, we use a 2.0 mm cannula. If we do not have it, we could use the more common 2.4 mm cannula, but we must handle it with care so as not to damage the articular surface.
reacae.31282.fs2401005en-figure6.png

Figure 6. Sequential preparation of the portals and positioning of the hands for triangulation. Transillumination visualization of the radial portal. Positioning of the 1.9 mm optics and synoviotome cannula. A pencil grip position using the third finger as a support on the patient's hand is usually a good method for achieving correct triangulation to help us perform an optimal technique and minimize the risk of iatrogenic articular cartilage damage.
Evacuation of the hematoma and debridement of the perilesional tissue
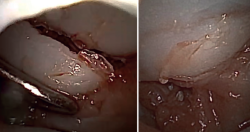
We begin complete evacuation of the fracture hematoma and the synovectomy. This allows inspection of the joint and better identification of the fracture pattern, as well as correct visualization of all the structures.
Inspection of the joint
To follow a reproducible systematic approach, we can start by visualizing the side opposite to where the arthroscope is inserted, i.e., the contralateral collateral ligament, and then assess the volar plate, identify the sesamoid bones (if any), the ipsilateral ligament, and finally the dorsal capsule. The metacarpal head and the base of the proximal phalanx are then assessed, followed by the synovial recesses and the origins of the collateral ligaments.
Identification of the type of fracture and fixation of the fragments
Once vision has improved, we can begin to assess the fracture pattern and can determine the plan for reduction and fixation.
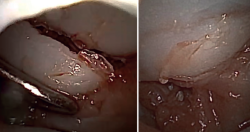
The free osteochondral fragments can be removed with grasping or mosquito forceps.
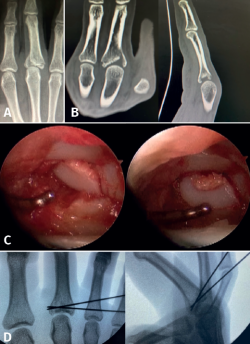
reacae.31282.fs2401005en-figure7.png
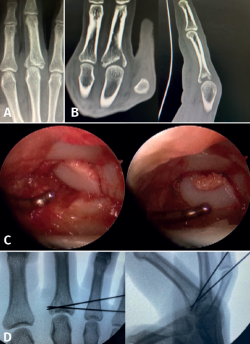
Figure 7. Comminuted fracture of the base of P1 of a third finger. Axial compression mechanism causing collapse of the osteochondral fragments. A: plain radiograph in anteroposterior projection; B: coronal and sagittal projections in computed tomography, which help us to study the fracture pattern, the number of fragments and their position; C: arthroscopic visualization of the articular surfaces. With the aid of the palpator, the fragments are reduced in sequence until adequate reduction of the articular surface is achieved; D: the osteochondral fragments are held in position by "joystick" placing of Kirschner wires, preventing the fragments from collapsing and thus maintaining joint congruence.
The main fragments are reduced with the aid of a palpator or a small blunt dissector. External reduction of the fragments may be necessary, especially when they are impacted in the centre of the articular surface. This is especially common at the base of the proximal phalanx. To do this, we introduce a 1.0 Kirschner wire through the fracture site, through an extra-articular "window", and in "joystick" fashion, we lower the impacted fragment. Sometimes it is advisable to check each of the maneuvers using fluoroscopy, which can be positioned perpendicular to the arm or in the traditional manner, which requires us to release the hand of the patient in order to perform the check.
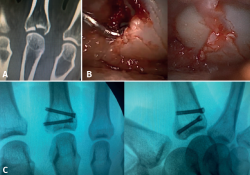
reacae.31282.fs2401005en-figure8.png
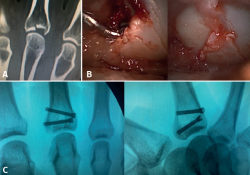
Figure 8. Fracture of the base of P1 of a third finger. Axial compression mechanism causing collapse of a central fragment. A: computed tomography images showing a large collapsed central fragment; B: arthroscopic visualization allows us to perform adequate reduction with the aid of a palpator and Kirschner wires through an extra-articular bony window; C: the size of the fragments and the characteristics of the fracture allow us to perform correct osteosynthesis with cannulated screws, which also accelerates the recovery process.
In some cases it is necessary to insert a spongy graft through the fracture site to maintain reduction and thus avoid joint step-off.
reacae.31282.fs2401005en-figure9.png
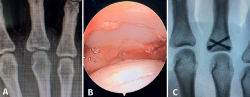
Figure 9. Fracture of the base of P1 of a third finger. Axial compression mechanism resulting in a joint fracture line with extra-articular extension. A: plain radiographic images showing the fracture pattern; B: arthroscopic visualization allows us to perform adequate reduction with the aid of a palpator and Kirschner wires through the fracture site; C: the size of the fragments and the characteristics of the fracture allow us to perform correct osteosynthesis with cannulated screws.
Once the fragments have been reduced, 0.8 or 1.0 Kirschner wires are used to maintain reduction (Figure 7). Sometimes we can only maintain reduction by applying a stop, to prevent the osteochondral fragment from collapsing. Depending on the fracture pattern and the surgeon's preference, we can use conventional screws, cannulated screws, etc. (Figures 8 and 9).
Postoperative management
The immobilization period will depend on the type and complexity of the fracture, the reduction we have obtained and the method of fixation used, as well as on the presence of associated soft tissue injuries, etc.
If a more or less prolonged period of immobilization is required, it will generally be done in flexion of the MCP joint to facilitate a tighter position of the collateral ligaments and thus allow better and earlier mobilization.
After initial management with or without immobilization, rehabilitation treatment plays a key role.
Complications
Fortunately, small joint arthroscopy has few complications. Most of them are the result of a poor surgical technique, which can lead to iatrogenic injuries.
These include damage to articular cartilage, tendons and nerve structures.
In order to avoid these problems, the use of specific equipment is necessary, as well as an important learning period, and careful handling of the instruments.
With regard to damage of the articular cartilage, we recommend the use of blunt trocars as well as 1.9 mm or smaller optics. Insertion into the joint cavity should be done with the aid of straight mosquito forceps, using gentle pressure, and intra-articular triangulation should be done with delicate maneuvering. A pencil grip position using the third finger as a support on the patient's hand is usually a good method to achieve this.
Complications from the use of radiofrequency have been reported, such as chondrolysis(1), damage to the joint capsule, the overlying extensor tendon or even the skin(5). Injuries of the flexor tendon have also been described, due to its proximity to the volar capsule.
To avoid these complications, authors employing radiofrequency advocate the use of a continuous saline or Ringer's saline irrigation system, as well as the use of intermittent transmission of the radiofrequency signal. In our experience, when performing dry arthroscopy, we also avoid the use of electrocautery, so we have not reported any injuries resulting from its use.
Injuries have also been reported as a result of preparation of the portals. Here we can observe nerve lesions of the cutaneous sensory branches and lesions of the extensor apparatus. Limosuin and Corella(3) conducted an anatomical study on the safety of arthroscopic portals and concluded that the third finger is the safest for the creation of portals, while the ulnar side of the second finger and the radial side of the fourth finger pose the highest risk of nerve injury(3).
To avoid nerve damage, it is advisable to make only a skin incision with a scalpel, followed by blunt penetration with straight mosquito forceps, according to our preference.
Due to the proximity of the extensor tendon to the portals, it is another structure susceptible to damage. To avoid this, care must be taken when inserting the instruments, and a controlled synovectomy under constant visualization must be performed.
Conclusions
Intra-articular fractures of the fingers are a clear indication for an arthroscopic procedure, which allows anatomical reduction and also minimizes the risk of joint fibrosis, reducing the recovery time and functional capacity of the joint.
To avoid potential complications, the use of specific equipment is necessary, together with an important learning period, and careful handling of the instruments.
Postoperative management will depend on the type of fracture, the reduction obtained, the method of osteosynthesis used, and the surgeon's preferences.
Figuras
Figure 1. Arthroscopic visualization of the metacarpophalangeal joint of a third finger. At the top of the image we see the base of the P1 with the corresponding fracture line. The metacarpal head is shown at the bottom of the image.
Figure 2. Fracture of the base of the proximal phalanx of a second finger due to ligamentous avulsion of the ulnar collateral ligament. In this case, arthroscopically assisted reduction, temporary fixation with Kirschner wires and cannulated screw osteosynthesis were performed.
Figure 3. Fracture of the base of the proximal phalanx of a second finger due to ligamentous avulsion of the ulnar collateral ligament. Direct visualization of the articular surface allows anatomical reduction to be made and correct positioning of the fragments to be checked after osteosynthesis.
Figure 4. Arrangement of an operating room in which small joint arthroscopy is performed using the Arthrex SynergyUHD4®arthroscopy tower.
Figure 5. Location and orientation of the portals on both sides of the extensor apparatus. Although the longitudinal orientation has been the reason why some authors advocate no need for stitches, we advise suturing of the portals at the end of the procedure. In the image, in addition to the portals, we see an accessory incision for the insertion of a cannulated screw.
Figure 6. Sequential preparation of the portals and positioning of the hands for triangulation. Transillumination visualization of the radial portal. Positioning of the 1.9 mm optics and synoviotome cannula. A pencil grip position using the third finger as a support on the patient's hand is usually a good method for achieving correct triangulation to help us perform an optimal technique and minimize the risk of iatrogenic articular cartilage damage.
Figure 7. Comminuted fracture of the base of P1 of a third finger. Axial compression mechanism causing collapse of the osteochondral fragments. A: plain radiograph in anteroposterior projection; B: coronal and sagittal projections in computed tomography, which help us to study the fracture pattern, the number of fragments and their position; C: arthroscopic visualization of the articular surfaces. With the aid of the palpator, the fragments are reduced in sequence until adequate reduction of the articular surface is achieved; D: the osteochondral fragments are held in position by "joystick" placing of Kirschner wires, preventing the fragments from collapsing and thus maintaining joint congruence.
Figure 8. Fracture of the base of P1 of a third finger. Axial compression mechanism causing collapse of a central fragment. A: computed tomography images showing a large collapsed central fragment; B: arthroscopic visualization allows us to perform adequate reduction with the aid of a palpator and Kirschner wires through an extra-articular bony window; C: the size of the fragments and the characteristics of the fracture allow us to perform correct osteosynthesis with cannulated screws, which also accelerates the recovery process.
Figure 9. Fracture of the base of P1 of a third finger. Axial compression mechanism resulting in a joint fracture line with extra-articular extension. A: plain radiographic images showing the fracture pattern; B: arthroscopic visualization allows us to perform adequate reduction with the aid of a palpator and Kirschner wires through the fracture site; C: the size of the fragments and the characteristics of the fracture allow us to perform correct osteosynthesis with cannulated screws.
Información del artículo
Cita bibliográfica
Autores
Iván Copete González
Servicio de Cirugía Plástica y Reconstructiva. Hospital Intermutual de Levante. Valencia
Unidad de Cirugía de Pie y Tobillo. Hospital Universitari i Politècnic La Fe. Valencia
Pedro Julián Jiménez Honrado
Servicio de Cirugía Plástica y Reconstructiva. Hospital Intermutual de Levante. Valencia
Unidad de Mano y Muñeca. Hospital Ribera IMSKE. Valencia
Ángel Navarro Monzonís
Servicio de Cirugía Plástica y Reconstructiva. Hospital Intermutual de Levante. Valencia
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Badia A. Arthroscopic Management of Metacarpophalangeal Articular Fractures. En: Bathia DN, Bain GI, Poehling GG, Graves BR (eds.). Arthroscopy and Endoscopy of the Elbow, Wrist and Hand. Springer; 2022. pp. 1117-26.
-
2Berger RA. Small-joint arthroscopy in the hand and wrist. En: Geissler WB (ed.). Wrist Arthroscopy. New York: Springer; 2005. pp. 155-66.
-
3Limousin B, Corella F, del Campo B, Fernández E, Corella MA, et al. Seguridad de los portales metacarpofalángicos. Estudio anatómico. Rev Esp Cir Ortop Traumatol. 2017;62(5):380-6.
-
4Rozmaryn LM, Wei N. Metacarpophalangeal arthroscopy. Arth- roscopy. 1999;15:333-7.
-
5Sekiya I, Kobayashi M, Okamoto H, Otsuka T. Progress and Role of Finger Joint Artrhoscopy. Hand Clin. 2017;33:819-29.
-
6Rozmaryn LM, Lamott K, Crawford P. Metacarpophalangeal arthroscopy: technique and indications. Tech Hand Up Extrem Surg. 2000;4(3):167-75.
-
7Berner SH. Metacarpophalangeal arthroscopy: technique and applications. Tech Hand Up Extrem Surg. 2008;12(4):208-15.
-
8Choi AK, Chow EC, Ho PC, Chow YY. Metacarpophalangeal joint arthroscopy: Indications revisited. Hand Clin. 2011;27:369-82.
-
9Lögters TT, Lee HH, Gehrmann S, Windolf J, Kaufmann RA. Proximal Phalanx Fracture Management. Hand (N Y). 2018;13(4):376-83.
-
10Piñal F. Dry Arthroscopy and its Applications. Hand Clin. 2011;27(3):335-45.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Learning from the best
- Everyone's effort
- Inclusion of the long portion of the biceps in rotator cuff repairs
- Surgical technique of the arthroscopic Latarjet procedure with button fixation
- Arthroscopic lateral collateral ligament plication of the elbow
- Arthroscopy-assisted treatment of metacarpophalangeal joint fractures of the fingers
- Surgical technique of hip arthroscopy without perineal post
- Direct reattachment in anterior cruciate ligament ruptures
- Application of fresh osteochondral allografts to the patella. Surgical procedure
- Arthroscopic ligamentoplasty for lateral ankle instability
- Two handles to grasp: double bucket-handle meniscal lesion
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.