Surgical technique of hip arthroscopy without perineal post
Técnica quirúrgica de artroscopia de cadera sin pivote perineal
Resumen:
El objetivo de este trabajo es describir la técnica de artroscopia de cadera sin uso de poste perineal. La artroscopia de cadera ha ganado popularidad en los últimos años como tratamiento para diversas patologías, aunque su realización no está exenta de complicaciones, algunas de ellas asociadas a la técnica quirúrgica utilizada, como es la neuroapraxia transitoria u otras más graves como hematomas y lesiones genitales, asociadas al uso de poste perineal. La técnica se realiza bajo anestesia general con relajación muscular continua, siendo imprescindible posicionar al paciente en decúbito supino sobre una almohadilla antideslizante. La luxación de la cadera se consigue mediante tracción axial, en posición de Trendelenburg. En nuestra experiencia, la técnica ha sido eficaz, reduciendo el número de complicaciones postoperatorias asociadas al uso de pivote central. Esta técnica es segura y fácilmente reproducible, además es económicamente viable, al solo precisar de una almohadilla antideslizante para su realización.
En esta técnica se proporcionan consejos y trucos obtenidos después de más de mil casos realizados por el cirujano senior, incluyendo recomendaciones específicas sobre la colocación del paciente, la realización de los portales, el manejo de la cápsula articular y el cierre capsular.
Abstract:
The present study describes the surgical technique of hip arthroscopy without the use of a perineal post. Hip arthroscopy has gained popularity in recent years as a treatment for different disorders, though it is not without complications. Some of these are related to the surgical technique used, such as transient neuropraxia or other more serious complications such as hematomas and genital injuries, associated with the use of a perineal post. The technique is performed under general anesthesia with continuous muscle relaxation, and the patient must be positioned in the supine position on a non-slip pad. Dislocation of the hip is achieved by axial traction, in the Trendelenburg position. In our experience, the technique has been effective, reducing the number of postoperative complications associated with the use of a central post. This technique is safe and easily reproducible, and is economically feasible, requiring only a non-slip pad.
The technique provides tips and tricks obtained after more than a thousand operations performed by the senior surgeon, including specific recommendations on patient positioning, the preparation of portals, joint capsule management, and capsule closure.
Introduction
Hip arthroscopy has gained popularity in recent years(1,2), establishing itself as an effective tool for the treatment of various hip disorders, and the number of indications is increasing rapidly. Despite the numerous techniques described for implementing hip arthroscopy, there is still no consensus on the most appropriate procedure for obtaining the best results.
Hip arthroscopy is not without risks, with reported complication rates ranging from 0.5-59%(3,4,5). An association has been observed between use of the perineal post and the occurrence of transient neuropraxia(6,7), as well as soft tissue injuries, and scrotal and vulvar tears(7,8). Perineal and inguinal dysesthesia rates of up to 41-59% have been reported when using a perineal post(9,10) . These complications are typically transient and resolve within days, weeks or months(11),although permanent lesions have also been reported(5). A systematic review by Habib et al.(7) reported an incidence of pudendal nerve injury of 1.8%.
To avoid these potential complications, hip dislocation techniques without the use of a post have gained popularity in recent years(12,13,14). The incorporation of new techniques represents a challenge for the surgeon, and is not without difficulties. In this article, we present a precise description of the technique we have been using in our center, with the basic set-up done in a way to make it easily reproducible in order to ensure satisfactory results.
Surgical technique
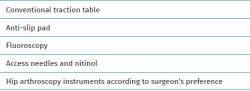
To perform this technique, collaboration with the anesthesia team is necessary to secure good relaxation of the patient, which will be crucial to achieve hip joint diastasis without the use of a perineal post generating resistance to axial traction of the limb. In our center, the anesthesia team uses a continuous intravenous infusion of rocuronium adjusted to the patient's weight: rocuronium bromide (Esmeron®) 0.5 mg/kg/h. We make sure that we have all the necessary equipment to perform the hip distraction surgical technique without the use of a perineal post. The list of required equipment is detailed in Table 1.
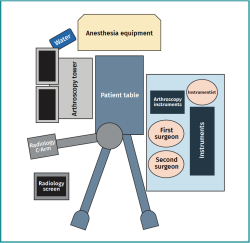
Operating room layout
In order to create a stable and comfortable surgical environment for the operation, we adopt a systematic room layout. This will allow us to have a sterile area where surgical techniques can be performed as comfortably as possible. Our proposed surgical layout is shown in Figure 1.
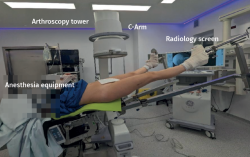
The patient is placed in supine decubitus on the traction table. The entire surgical team is positioned on the side where the operation is to be performed. This will provide a closed sterile area to work in (Figure 2).
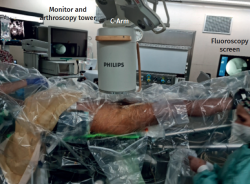
On the opposite side, from cranial to caudad, we place the support of the fluids that provide the necessary flow to perform hip arthroscopy. Next, we position the suction pump and the arthroscopy tower with the equipment screens directly in front of the surgeon for comfortable and close viewing. Then, the image intensifier arm is positioned, entering from the opposite side and which will be free to move according to the needs of the surgery. In addition, the radioscopy screen should be placed close to the patient's feet so that the surgical team has a direct, unobstructed field of view (Figure 3).
Positioning of the patient
Once the patient is intubated and relaxed, we proceed to position him/her. The patient should lie supine on a non-slip pad correctly placed on the operating table (Figure 4). In our center we use an anti-slip pad (CarePad®) made of high-density viscoelastic material to ensure even distribution of the patient pressure. It is essential to avoid surgical pyjamas and sheets, to ensure full contact between the pad and the skin of the gluteal and lumbar region in order to generate sufficient resistance to allow the patient to adhere to the surgical table. For reference, the patient's position is similar to that obtained with the use of a post.
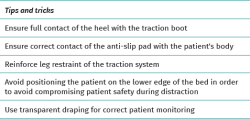
Once the patient is in a satisfactory position, we place both legs in the traction system available in our operating room, checking that both heels are correctly positioned. We use self-adhesive elastic bandaging to reinforce the traction system. For the upper extremities, we cross the patient's arm on the surgical side over the chest, using a suitably padded support to avoid any compression. The contralateral arm is placed in an arm support, facilitating access to the different lines needed for drug administration of the patient during the operation. We recommend the use of a transparent drape so that signs of abdominal extravasation can be monitored at all times (Figure 5 and Table 2).
Hip distraction
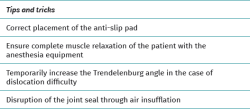
We perform hip distraction under radiological control to ensure easy entry of the different arthroscopic portals at the start of surgery. We ensure that the image is correctly centered over the hip joint. It is essential to place the patient in10-15° Trendelenburg to provide a gravity force vector together with the anti-slip pad, sufficient for hip dislocation (Figure 4). It is important to consider the weight of the patient. The heavier the patient, the less Trendelenburg will be required, while very light-weight patients may require more Trendelenburg to counteract axial traction. The contralateral leg is abducted approximately 10-20° and positioned with minimal traction to balance the traction force on the leg to be operated upon.
Initially, traction is applied with the limb in maximum abduction, and subsequently it is brought into neutral abduction. This maneuver often secures sufficient distraction. If not, axial traction is added with the operating table tractor system. Traction is performed in internal rotation to counteract femoral anteversion and to be able to work in a horizontal plane. Fluoroscopic control must ensure distraction that allows us to create the arthroscopic portals safely. Occasionally, we may hear a clicking sound when distraction of the hip joint is achieved, indicating that the natural seal has been lost, in the case of a competent acetabular labrum. Once sealing is lost, the Trendelenburg position can usually be decreased to maintain joint distraction. If sufficient distraction is not achieved on the first attempt, we ensure that the patient is properly relaxed and repeat the maneuver, temporarily increasing the Trendelenburg degrees to20-30° if necessary (Figure 6).
Another technique we can use to facilitate distraction is disruption of the joint seal by insufflating air (30 ml) into the joint with an 18 gauge needle under radiological control, after initial traction. This will create a positive pressure within the joint capsule, eliminating the native negative pressure, and thus facilitating further distraction of the joint. The insufflation of air into the joint will allow us to check that we are inside the joint by delimiting a radiolucent area corresponding to the joint capsule (Table 3).
Arthroscopic portals
For hip arthroscopy, we use the inside-out technique, with minor modifications. We systematically use the anterolateral (AL) and modified mid-anterior portals (mMAP) and, if necessary, a third portal is established: the distal anterolateral accessory portal (DALA).
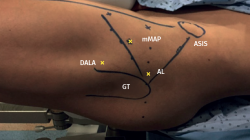
We start the surgery by identifying the different anatomical points that will guide us during creation of the arthroscopic portals. First, we locate the anterosuperior iliac spine (ASIS) and the patella, drawing a line connecting these two points that will serve as our surgical boundary. It is essential to avoid exceeding this limit medially in order to avoid damaging the adjacent vascular structures. Next, we identify the greater trochanter (GT) and mark the AL portal at its anterosuperior margin. It is advisable for this portal to be located as close as possible to the trochanter in order to facilitate access to the joint. The mMAP is then marked approximately 7 cm or 4 fingers from the AL portal in an anterior and medial direction and at45° in a craniocaudal direction. Finally, we place the DALA portal at an equidistant distance between the AL portal and the mMAP, forming an equilateral triangle (Figure 7).
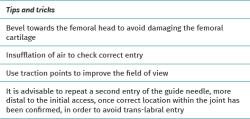
We perform the AL arthroscopic portal under fluoroscopic control to confirm positioning of the guide needle. The guide is inserted with the bevel facing towards the femoral head in order to avoid damaging the cartilage of the latter. We visualize the location of the coxofemoral joint seeking to triangulate the entry point so that we access from the most lateral part of the acetabulum. To do this, we can imagine a line halfway between the pubis and the ASIS. As a general rule, the guide needle is oriented about20° in the cephalic direction. If we have adequately corrected the patient's femoral anteversion with internal rotation of the leg, as explained above, we should be able to enter with a direction parallel to the ground. By palpation, we detect the initial resistance of the fascia lata and, secondly, the resistance of the joint capsule, identifying the entry in the joint. We check the intra-articular location through palpation with nitinol wire (with blunt ends), touching with the acetabular fundus and via radioscopy control. We insufflate 30 ml of air to help us identify the rim of the acetabular labrum and physiological communication with the psoas - this being important to prevent possible abdominal fluid extravasation (Figure 8). To minimize the risk of trans-labral penetration, it is advisable to consider removing the guide needle after air insufflation and re-enter while taking care to avoid the footprint of the acetabular labrum (Table 4).
The mMAP is performed under direct visualization of the arthroscopic triangle formed by the acetabular labrum, the femoral head, and the limit of view of the arthroscope, in the anterior region of the joint. Finally, if necessary, we establish the DALA portal likewise under direct visualization.
Capsulotomy
To ensure optimal visualization and in order to work comfortably, we perform the interportal capsulotomy. Only this measure will guarantee comfortable, safe and complete access to the entire anterior and lateral acetabular region for the proper assessment and treatment of possible lesions. After performing the mMAP, we switch the viewing camera to the mMAP so that we can visually check the exact location of our AL portal and, if it seems correct, we start the interportal capsulotomy. If a trans-labral portal has been made, we correct it and evaluate whether the lesion produced needs to be repaired (this is usually not the case, since the orifice measures 5 mm). Once the interportal capsulotomy has been started, we again switch the arthroscope to the AL portal to complete the capsulotomy from mMAP. To approach the peripheral compartment, after the removal of traction and placement of the limb at40° of hip flexion, we expand the capsulotomy by making a "T" shaped incision, where the interportal capsulotomy will be the top part of the "T". For this purpose, it is useful to place traction stitches in the capsule, thus allowing the capsulotomy to be performed evenly and safely.
To improve visibility during surgery, it is advisable to use well-placed traction points, which will allow us to maintain constant traction in the form of a tent, thus widening our field of view(15). This is achieved by placing a suture through the capsular ridge in the desired position, pulling from outside and applying mosquito grasping forceps over the skin to maintain the traction obtained.
Capsule closure
Once the surgery has been performed, capsule closure is carried out. To do this, we start the closure with stitches from distal to proximal of the vertical arm of the "T", followed by one or two stitches of the interportal capsulotomy, being careful not to include the reflex portion of the rectus femoris in this repair.
Discussion
Hip arthroscopy is a complex surgical technique with a long learning curve, making it a challenge for surgeons to master the technique. In order to speed up this learning curve, we present the technique that we use in our center on a routine basis, and which represents the technical evolution that has given us the best results after more than 20 years dedicated to hip arthroscopy.
The gold standard in arthroscopic hip surgery includes a counter-traction post. However, several techniques without a post have been described(12,13,15,16), although they are still in minority use. Fletcher et al.(17) propose external fixation with threaded pins inserted into the femoral diaphysis and acetabulum. With this method, the authors reported no neurological complications in a series of 23 patients. However, the use of these pins has its own complications, including iatrogenic fractures, infections and increased postoperative pain. Mei-Dan et al.(18) in turn describe the use of a post at thigh level, about 10 cm from the perineum. In over 2000 patients, the authors reported no complications related to the inguinal zone or perineum; however, they have described other possible complications such as obturator nerve neuropraxia.
The reported complication rates associated with the use of a perineal post vary widely from 0.05-59%(4,5,19,20). Pudendal nerve palsy is the most common complication described after perineal post hip arthroscopy(8,20,21). The most widely accepted interpretation of nerve injury as a complication of hip arthroscopy is the combination of traction and compression forces. A study in cadavers revealed a significant increase in pressure with increasing traction force in the ischial tuberosity and genital region, suggesting that pudendal nerve injury may be due to compressive rather than traction force(22).
In a systematic review of 92 studies with 6134 patients, Harris et al.(21) showed the most frequent complication, along with iatrogenic chondrolabral injury, to be pudendal neuropraxia after hip arthroscopy. In this systematic review, perineal lesions were described in a total of 10 cases (0.16%). Kreautler et al.(23) have conducted a prospective comparative study of systems with an inguinal post versus systems without a post. The authors found a significantly lower risk of inguinal dysesthesias secondary to pudendal neuropraxia in the group without a post (0 versus 30%; p < 0.0001). They also reported a decreased risk of peroneal nerve neuropraxia in the group without a post (12 versus 32%; p = 0.04).
Different techniques have been described for distraction of the hip joint without the use of an inguinal post. Mei-Dan et al.(18), in a prospective cohort study of 1000 hip arthroscopies, described a technique that combines the Trendelenburg position with the use of a specific traction system to achieve hip distraction without the use of a perineal post. The technique we present focuses on eliminating the use of the perineal post to obtain hip joint distraction by simply using an additional anti-slip pad(13), which hardly increases the costs of surgery.
In our experience, we have seen that patients with a low body mass index may present greater difficulties during surgical preparation. In these cases, the patient's weight may not be sufficient to ensure adequate friction with the anti-slip pad, thus potentially making dislocation of the hip joint more difficult. We recommend initially increasing the degree of Trendelenburg to about30° to improve the gravitational force exerted on the pad and thus facilitate joint dislocation (Figure 6)(24). In addition, patients with pincer-type morphology or with some degree of coxarthrosis may pose additional challenges at the time of joint dislocation. In such cases, it is often wiser to access the peripheral compartment in the first instance or adopt an outside-in approach. However, in our experience, this is much more traumatic to the joint and may cause us to reconsider the benefits of the preservation surgery we are about to perform.
Among the possible limitations of hip distraction techniques without the use of a perineal post, mention must be made of the need for the Trendelenburg position. Theoretically, a Trendelenburg position maintained throughout an operation could alter venous flow of the operated limb. In a prospective study involving a cohort of 35 patients, Welton et al.(24) observed no significant reduction in venous flow in the common femoral or popliteal veins. Another possible complication of hip arthroscopy is fluid extravasation. However, the literature has not reported an association between this complication and use of the technique without a perineal post(25).
When performing the arthroscopic portals, we must ensure that adequate distraction of the joint has been achieved. The identification of the different anatomical points will help us to secure optimal access points. Poor positioning of the arthroscopic portals can affect the rest of the surgery. We therefore must take the time necessary to obtain adequate access to allow proper visualization and maneuverability during the operation. Each surgeon has his or her own preferences or a variation of portals to suit personal comfort, but the AL portal, described by Burman in 1931, remains the initial portal in most cases for accessing the central compartment of the hip(26).
Capsulotomy is essential to ensure adequate maneuverability during surgery. However, capsulotomy is controversial due to possible iatrogenic damage to the joint capsule, especially to the iliofemoral ligament(27). A sufficiently wide capsulotomy must be performed to avoid damaging it during our surgical technique and to ensure proper repair of the capsule at the end of the procedure. We seek to restore the previous anatomy of the hip joint through precise capsule closure. As Bakshi et al. point out(28), sacrifice of the stabilizing ligaments of the hip joint could lead to hip instability with anterior hip displacement. Despite the controversies, recent research shows superior results in terms of patient reported outcomes (PROs) with capsule closure(19,29,30).
Conclusions
Hip arthroscopy without the use of a perineal post is an effective, reproducible and safe technique that significantly reduces the incidence of complications related to the use of a post.
Supplementary material
The video accompanying this article can be seen at (Video 1):
Tablas
Figuras
Figure 4. Final positioning of the patient prior to joint distraction. We ensure correct contact with the anti-slip pad. The patient is placed in 10-15° Trendelenburg.
Figure 5. Final positioning of the patient prior to the start of surgery. We use a transparent drape that will allow adequate monitoring of the patient and facilitate the identification of any extravasation.
Figure 6. Proposed technique to achieve dislocation of the coxofemoral joint in complex cases. The Trendelenburg angle is temporarily increased to 30°, maximum abduction is performed, and the leg is placed in slight hip flexion, thus obtaining traction with a greater force vector.
Figure 7. View of a left hip with drawing of the different anatomical references. AL: anterolateral portal; mMAP: modified mid-anterior portal; DALA: distal anterolateral portal; GT: greater trochanter; ASIS: anterosuperior iliac spine.
Figure 8. A: insertion of the guide needle from the anterolateral portal, ensuring that the bevel is oriented towards the femoral head; B: delineation of the radiolucent capsular contour by insufflating air into the joint to check that we are inside it.
Información del artículo
Cita bibliográfica
Autores
Josep Ferrer Rivero
MC-Mutual Barcelona
I-Move Traumatologia. Barcelona
Robert Ferrer Rivero
Hospital Sant Rafael. Barcelona
Cristina Requena Ribas
Hospital Germans Trias i Pujol. Badalona
Joan Cabello Gallardo
Imove Traumatología. Barcelona
Hospital Germans Trias i Pujol. Badalona
Grupo Ibérico de Preservación de Cadera (GIPCA)
Xavier Lizano Diez
I-Move Traumatologia. Barcelona
Hospital del Mar. Barcelona
Marc Tey Pons
Unidad de Cadera. iMove Traumatología. Hospital Mi Tres Torres. Barcelona
I-Move Traumatologia. Barcelona
Hospital Universitari Parc Taulí. Sabadell
Grupo Ibérico de Preservación de Cadera (GIPCA)
Universidad Pompeu Fabra
Unidad de Cadera. Servicio de Cirugía Ortopédica y Traumatología. Hospital del Mar. Barcelona
Unidad de Artroscopia y Rodilla. ICATME-Institut Universitari Dexeus. Universitat Autònoma de Barcelona
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed, and that all the patients included in the study have received sufficient information and have given written informed consent to participation in the study.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Zusmanovich M, Haselman W, Serrano B, Banffy M. The Incidence of Hip Arthroscopy in Patients With Femoroacetabular Impingement Syndrome and Labral Pathology Increased by 85% Between 2011 and 2018 in the United States. Arthroscopy. 2022;38(1):82-7.
-
2Schairer WW, Nwachukwu BU, Suryavanshi JR, Yen YM, Kelly BT, Fabricant PD. A Shift in Hip Arthroscopy Use by Patient Age and Surgeon Volume: A New York State–Based Population Analysis 2004 to 2016. Arthroscopy. 2019;35(10):2847-2854.e1.
-
3Dippmann C, Thorborg K, Kraemer O, Winge S, Hölmich P. Symptoms of Nerve Dysfunction After Hip Arthroscopy: An Under-Reported Complication? Arthroscopy. 2014;30(2):202-7.
-
4Zeman P, Rafi M, Kautzner J. Evaluation of primary hip arthroscopy complications in mid-term follow-up: a multicentric prospective study. Int Orthop. 2021;45(10):2525-9.
-
5Harris JD, McCormick FM, Abrams GD, et al. Complications and Reoperations During and After Hip Arthroscopy: A Systematic Review of 92 Studies and More Than 6,000 Patients. Arthroscopy. 2013;29(3):589-95.
-
6Park MS, Yoon SJ, Kim YJ, Chung WC. Hip Arthroscopy for Femoroacetabular Impingement: The Changing Nature and Severity of Associated Complications Over Time. Arthroscopy. 2014;30(8):957-63.
-
7Habib A, Haldane CE, Ekhtiari S, et al. Pudendal nerve injury is a relatively common but transient complication of hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):969-75.
-
8Gupta A, Redmond JM, Hammarstedt JE, Schwindel L, Domb BG. Safety Measures in Hip Arthroscopy and Their Efficacy in Minimizing Complications: A Systematic Review of the Evidence. Arthroscopy. 2014;30(10):1342-8.
-
9Mas Martínez J, Sanz-Reig J, Morales Santias M, Martínez Gimenez E, Bustamante Suarez de Puga D, Verdu Román C. Femoroacetabular impingement: prospective study of rate and factors related for nerve injury after hip arthroscopy. J Orthop. 2019;16(5):350-3.
-
10Reda B, Wong I. Postoperative Numbness: A Survey of Patients After Hip Arthroscopic Surgery. Orthop J Sports Med. 2018;6(5).
-
11Polyzois I, Tsitskaris K, Oussedik S. Pudendal nerve palsy in trauma and elective orthopaedic surgery. Injury. 2013;44(12):1721-4.
-
12Kollmorgen RC, Ellis T, Lewis BD, Harris JD. Achieving Post-Free Distraction in Hip Arthroscopy With a Pink Pad Patient Positioning Device Using Standard Hip Distraction Tables. Arthrosc Tech. 2019;8(4):e363-8.
-
13Perry AK, Gursoy S, Singh H, Vadhera AS, Mehta N, Chahla J. The Pink Pad: A Method of Post-Free Distraction During Hip Arthroscopy. Arthrosc Tech. 2021;10(8):e1897-902.
-
14Jiménez ML, Haneda M, Pascual-Garrido C. The Hip Arthroscopy Post-less Procedure Impingement (HAPPI) Technique: Achieving Distraction With Standard Hip Tables at Zero Additional Cost. Arthrosc Tech. 2020;9(11):e1697-701.
-
15Salas AP, Mazek J, Araújo-Reyes D, González-Campos M, Castillo-Trevizo A, García JM. The Tutankhamun Technique in Hip Arthroscopy. Arthrosc Tech. 2018;7(11):e1167-71.
-
16Welton KL, Garabekyan T, Kraeutler MJ, et al. Effects of Hip Arthroscopy Without a Perineal Post on Venous Blood Flow, Muscle Damage, Peripheral Nerve Conduction, and Perineal Injury: A Prospective Study. Am J Sports Med. 2019;47(8):1931-8.
-
17Flecher X, Dumas J, Argenson JN. Is a hip distractor useful in the arthroscopic treatment of femoroacetabular impingement? Orthop Traumatol Surg Res. 2011;97(4):381-8.
-
18Mei-Dan O, McConkey MO, Young DA. Hip Arthroscopy Distraction Without the Use of a Perineal Post: Prospective Study. Orthopedics. 2013;36(1).
-
19Riff AJ, Kunze KN, Movassaghi K, et al. Systematic Review of Hip Arthroscopy for Femoroacetabular Impingement: The Importance of Labral Repair and Capsular Closure. Arthroscopy. 2019;35(2):646-56.e3.
-
20Dippmann C, Thorborg K, Kraemer O, Winge S, Hölmich P. Symptoms of Nerve Dysfunction After Hip Arthroscopy: An Under-Reported Complication? Arthroscopy. 2014;30(2):202-7.
-
21Harris JD, McCormick FM, Abrams GD, et al. Complications and Reoperations During and After Hip Arthroscopy: A Systematic Review of 92 Studies and More Than 6,000 Patients. Arthroscopy. 2013;29(3):589-95.
-
22Wininger AE, Kraeutler MJ, Goble H, Cho J, Mei-Dan O, Harris JD. The Physics of Postless Hip Arthroscopy. Arthrosc Tech. 2024;13(10):103077.
-
23Kraeutler MJ, Fasulo SM, Dávila Castrodad IM, Mei-Dan O, Scillia AJ. A Prospective Comparison of Groin-Related Complications After Hip Arthroscopy With and Without a Perineal Post. Am J Sports Med. 2023;51(1):155-9.
-
24Decilveo AP, Kraeutler MJ, Dhillon J, et al. Postless Arthroscopic Hip Preservation Can be Adequately Performed Using Published Techniques. Arthrosc Sports Med Rehabil. 2023;5(1):e273-80.
-
25Decilveo AP, Kraeutler MJ, Dhillon J, et al. Postless Arthroscopic Hip Preservation Can be Adequately Performed Using Published Techniques. Arthrosc Sports Med Rehabil. 2023;5(1):e273-80.
-
26Magrill ACL, Nakano N, Khanduja V. Historical review of arthroscopic surgery of the hip. Int Orthop. 2017;41(10):1983-94.
-
27Lee H, Lim W, Lee S, Jo S, Jo S. Impact of Capsulotomy on Hip Biomechanics during Arthroscopy. Medicina (B Aires). 2022;58(10):1418.
-
28Bakshi NK, Bayer JL, Bigelow EMR, Jameel OF, Sekiya JK. The Effect of Capsulectomy on Hip Joint Biomechanics. Orthop J Sports Med. 2017;5(10).
-
29Nho SJ, Beck EC, Kunze KN, Okoroha K, Suppauksorn S. Contemporary Management of the Hip Capsule During Arthroscopic Hip Preservation Surgery. Curr Rev Musculoskelet Med. 2019;12(3):260-70.
-
30Looney AM, McCann JA, Connolly PT, Comfort SM, Curley AJ, Postma WF. Routine Capsular Closure With Hip Arthroscopic Surgery Results in Superior Outcomes: A Systematic Review and Meta-analysis. Am J Sports Med. 2022;50(7):2007-22.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Learning from the best
- Everyone's effort
- Inclusion of the long portion of the biceps in rotator cuff repairs
- Surgical technique of the arthroscopic Latarjet procedure with button fixation
- Arthroscopic lateral collateral ligament plication of the elbow
- Arthroscopy-assisted treatment of metacarpophalangeal joint fractures of the fingers
- Surgical technique of hip arthroscopy without perineal post
- Direct reattachment in anterior cruciate ligament ruptures
- Application of fresh osteochondral allografts to the patella. Surgical procedure
- Arthroscopic ligamentoplasty for lateral ankle instability
- Two handles to grasp: double bucket-handle meniscal lesion
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.