Extraarticular plasty as sole maneuver in the correction of rotational instability due to rupture of the anterior cruciate ligament in an elderly patient
Plastia extraarticular como gesto único en la corrección de la inestabilidad rotacional por rotura del ligamento cruzado anterior en un paciente de edad avanzada
Resumen:
Históricamente, los pacientes mayores de 45 años con rotura del ligamento cruzado anterior (LCA) no se han considerado subsidiarios de cirugía. Cada vez son más los autores que consideran la reconstrucción en pacientes con inestabilidad sintomática, independientemente de la edad. La plastia extraarticular tiene menor tiempo de recuperación, proporcionando una mejoría de la inestabilidad rotacional, principal causa de episodios de fallo en pacientes con rotura del LCA.
Se presenta el caso de una paciente de 67 años con rotura del LCA que, tras realizar tratamiento conservador, presentaba múltiples episodios de inestabilidad rotacional con Lachman positivo y un pivot-shift explosivo. Se realizó una plastia extraarticular anterolateral aislada de Lemaire modificada con doble fijación (tornillo interferencial y sistema de suspensión).
La plastia extraarticular es una técnica con menor tiempo de recuperación que la plastia intraarticular, proporcionando una mejoría de la inestabilidad rotacional. La fijación puede adaptarse en cada paciente, realizando doble fijación en aquellos casos que presenten baja calidad ósea. Es una opción que tener en cuenta en pacientes de avanzada edad con rotura sintomática del LCA.
Nivel de evidencia: IV.
Abstract:
Historically, patients over 45 years of age with rupture of the anterior cruciate ligament (ACL) have not been considered candidates for surgery. An increasing number of authors are considering reconstruction in patients with symptomatic instability, independently of age. Extraarticular plasty is associated with faster recovery, affording improvement of rotational instability, which is the main cause of failure episodes in patients with rupture of the ACL.
We present the case of a 67-year-old woman with rupture of the ACL, who after conservative management suffered multiple episodes of rotational instability with a positive Lachman test and explosive pivot-shift. Isolated modified Lemaire anterolateral extraarticular plasty was performed, with double fixation (interference screw and suspension system).
Extraarticular plasty is associated with faster recovery than intraarticular plasty, affording improvement of the rotational instability. Fixation can be adapted to each patient, performing double fixation in those cases where bone quality is poor. It is an option to be taken into account in elderly patients with symptomatic rupture of the ACL.
Level of evidence: IV.
Introduction
Insufficiency of the anterior cruciate ligament (ACL) produces anteroposterior and rotational instability - with the latter being less tolerated by the patient. With isolated intraarticular plasty, pivot-shift control is relatively ineffective, as the structure is located close to the axis of rotation of the knee (1). In recent years there has been an increase in the percentage of cases where this type of reconstruction is combined with extraarticular plasty of the anterolateral ligament, in view of the risk of residual rotational instability(2). Patients with symptomatic instability due to ACL rupture are amenable to surgical treatment, regardless of their age(3). Isolated anterolateral extraarticular tenodesis may prove sufficient in low functional demand elderly patients with symptomatic instability.
Clinical case
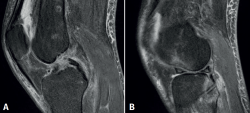
We present the case of a 67-year-old woman with ACL rupture following direct trauma 5 years ago. Considering her age and sedentary lifestyle, with no sports activity of any kind, conservative management was decided. Since the time of injury, she had experienced multiple rotational instability episodes, with increasingly frequent falls. Because of this, the patient had visited several specialists, who disadvised surgical treatment. The latest knee instability episode resulted in fracture of the distal radius, which was treated on a conservative basis. The exploration evidenced anteroposterior and rotational instability with a positive Lachman test and explosive pivot-shift. The patient suffered pain at the posteromedial joint line. The magnetic resonance imaging study evidenced ACL rupture with bone edema in areas inherent to acute instability episodes (anterolateral femoral condyle and posterolateral tibial plateau) (Figure 1)(4). Rupture of the external meniscus was also noted, with suspected injury of the posterior ramp of the internal meniscus.
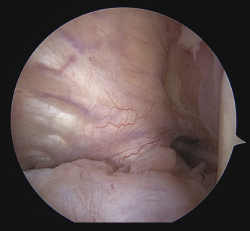
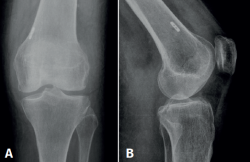
The arthroscopic exploration confirmed rupture of the ACL (Figure 2) and both menisci, while rupture of the posterior ramp of the internal meniscus was discarded via trans-notch access to the posteromedial compartment. The external meniscus showed complex rupture combining a radial portion and cleavage rupture of the body with defibrillation of the anterior horn. Partial resection was carried out until a stable margin was obtained, and all-inside suturing was performed with two circumferential vertical stitches using FiberStitch® (Arthrex, Naples, FL, USA) and outside-in circumferential sutures with number 0 non-reabsorbable material (FiberWire®, Arthrex, Naples, FL, USA) in the anterior horn zone. The internal meniscus presented a vertical longitudinal rupture measuring about 8 mm in length, in red zone, of the posterior horn, that was sutured with two vertical stitches using FiberStitch®, after percutaneous needle release of the medial collateral ligament(5) (Figure 3). Following the repair of both menisci, a modified Lemaire anterolateral extraarticular plasty was performed(2). Based on an incision measuring about 3 cm in length and centered on the lateral collateral ligament (LCL), a 1-cm wide iliotibial band plasty was performed and, keeping its distal insertion in Gerdy's tubercle, proximal sectioning was made at a distance of 9 cm (Figure 4). The plasty was enveloped in padding soaked with vancomycin(6). The plasty insertion point was located 1 cm proximal and posterior to the lateral epicondyle, and a guide needle was inserted using the hands free technique, with a 20º cranial and 20º proximal orientation. Then, a drill measuring 5 mm in diameter (Arthrex, Naples, FL, USA) was advanced until the medial cortical stop was reached, without penetrating through it, ensuring a tunnel of sufficient length. Sliding of the reinforced plasty with high resistance sutures (FiberLoop 2®, Arthrex, Naples, FL, USA) beneath the LCL was carried out, establishing a pulley and inserting and fixing it in the femoral tunnel. Due to the subjective impression of poor bone quality during drilling of the tunnel, we performed double fixation using a cortical suspension system(TightRope® with FiberTag®, Arthrex, Naples, FL, USA), combined with a PEEK® interference screw measuring 6 × 23 mm (Arthrex, Naples, FL, USA). Adequate positioning of the suspensory cortical button was checked through direct arthroscopic visualization in the extraarticular space from the anteromedial portal at the time of the flipping maneuver (Figure 5). Fixation of the plasty was made in full extension. The control radiographs showed correct positioning of the femoral tunnel and cortical fixation device (Figure 6).
The postoperative recommendations included Game Ready® cryotherapy-compression therapy (Alpharetta, GA, USA), and active ankle and isometric quadriceps exercises. Immobilization of the lower extremity was not indicated. Immediate weight bearing and walking with the help of two crutches was allowed(7). Flexion was limited to 60º during the first two weeks, and was then gradually increased to full flexion. The postoperative control visits evidenced an excellent clinical course, with full range of motion and walking without limping after two weeks. Pivot-shift proved negative 39 months after the operation. The Lachman test remained slightly positive. The patient was able to lead her normal life without limitations or pain. The scores on the Tegner (2) and Lysholm scales (95) were the same as before ACL rupture. She reported no new instability episodes or falls, and was very satisfied with the outcome (subjective assessment of the clinical evolution 9/10).
reacae.30380.fs2206010en-figure3.png
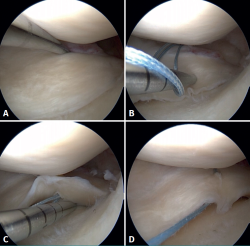
Figure 3. View of the internal compartment from the anterolateral portal of the left knee. All-inside suturing with vertical stitches. A: vertical longitudinal rupture measuring about 8 mm in length, in red zone, of the posterior horn of the internal meniscus; B: first anchoring of the all-inside suture; C: second anchoring of the all-inside suture. Tightening of the suture and closing of the gap; D: tightening of the self-locking sliding knot.
Discussion
Based on the present case, isolated extraarticular tenodesis may prove sufficient to control the subjective instability symptoms of elderly patients with ACL rupture. In patients over 45 years of age there is a tendency to prescribe conservative management of ACL ruptures. Approximately one-third of these patients recover their previous function; a similar proportion adapt their activities; and the remaining third finally required surgery due to recurrent instability episodes(8). In those cases where conservative management fails, surgery is indicated within a longer time interval than in younger patients(9). Despite the belief that the outcomes of reconstruction in patients of this kind may be conditioned by degenerative changes at chondral or meniscal level, recent studies have reported results comparable to those obtained in younger individuals(9,10). The percentage of complications is similar in both groups, though younger individuals recover faster.
Intraarticular plasties take longer to integrate, due to synovial fluid reflux in the bone tunnel - a factor that is independent of age - while more elderly patients additionally have a lower revascularization rate, with slower postoperative rehabilitation(2,11). Thus, in cases such as that described in the present study, isolated extraarticular plasty may be decided. Extraarticular plasties of this kind have always been subject to controversy, and became no longer used as a first option in view of the good clinical outcomes afforded by intraarticular plasties(12). There has been renewed interest in techniques of this kind in recent years, as biomechanical studies have seen that no intraarticular plasties - not even the bifascicular protocols - are able to full control pivot-shift(1,13,14). An isolated extraarticular plasty stabilizes the knee at rotational level by avoiding subluxation of the external tibial plateau, with practically no impact upon the Lachman test(15). Given the age and low functional demands of the patient, we consider the outcome obtained to be acceptable, since under-correction in anteroposterior translation is better tolerated and produces less instability sensation than residual rotational instability(8,16). Postoperative pivot-shift compared with the Lachman test produces more instability episodes with knee rotation and flexion defects, limitation of sports performance and activities of daily living, with lower scores on the Lysholm scale(17). In patients with poor bone quality, double fixation can be performed, combining a suspensory system with an interference screw. In any case, the current evidence is limited as regards the superiority of one technique over the other, as well as concerning the choice of combined fixation(18).
Conclusions
In elderly patients with low functional demands that present symptomatic rotational instability secondary to ACL rupture, isolated extraarticular plasty may be a treatment option, with less surgical aggression and faster patient recovery.
Figuras
Figure 1. Magnetic resonance imaging sagittal sections of the left knee. A: rupture of the anterior cruciate ligament; B: bone edema in the anterior region of the external femoral condyle and posteroexternal tibial plateau secondary to a rotational instability episode.
Figure 2. Arthroscopic view of the intercondylar notch (left knee), showing the absence of the anterior cruciate ligament secondary to chronic rupture.
Figure 3. View of the internal compartment from the anterolateral portal of the left knee. All-inside suturing with vertical stitches. A: vertical longitudinal rupture measuring about 8 mm in length, in red zone, of the posterior horn of the internal meniscus; B: first anchoring of the all-inside suture; C: second anchoring of the all-inside suture. Tightening of the suture and closing of the gap; D: tightening of the self-locking sliding knot.
Figure 4. Intraoperative view of the left knee. Patient in supine decubitus, with left lower extremity in knee support. Note the iliotibial band plasty measuring 1 cm in width and 9 cm in length, reinforced with high-resistance suture.
Figure 5. Intraoperative view of the left knee. A: patient in supine decubitus, with the left lower extremity in extension, and arthroscopic visualization of the extraarticular space from the anteromedial portal; B: direct control of correct flipping of the cortical suspension system.
Información del artículo
Cita bibliográfica
Autores
María Arnaudas Casanueva
Hospital Universitario Miguel Servet. Zaragoza
Beatriz Fernández Maza
Hospital Universitario Puerta de Hierro-Majadahonda. Madrid
Hospital Universitario HM-Torrelodones. Madrid
Diego García-Germán Vázquez
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario HM Torrelodones. Universidad San Pablo CEU. Torrelodones. Madrid
Clínica DKF. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Central de la Cruz Roja San José y Santa Adela. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Puerta de Hierro-Majadahonda. Majadahonda. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Williams A, Ball S, Stephen J, White N, Jones M, Amis A. The scientific rationale for lateral tenodesis augmentation of intra-articular ACL reconstruction using a modified ‘Lemaire’ procedure. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1339-44.
-
2García-Germán Vázquez D, Gómez Cáceres A, Occhi Gómez B. Tenodesis Extrarticular de Lemaire Modificada. En: Gómez Cáceres A, García-Germán D, Espejo Reina A. Ligamento Anterolateral de la Rodilla. Editorial Académica Española; 2018 pp. 1-8.
-
3Iorio R, Iannotti F, Ponzo A, Proietti L, Redler A, Conteduca F. Anterior cruciate ligament reconstruction in patients older than fifty years: a comparison with a younger age group. Int Orthop. 2018;42(5):1043-9.
-
4Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med. 2014;44:281-93.
-
5Claret G, Montañana J, Ríos J, et al. The effect of percutaneous release of the medial collateral ligament in arthroscopic medial meniscectomy on functional outcome. Knee. 2016;23(02):251-5.
-
6Pérez-Prieto D, Torres-Claramunt R, Gelber PE, Shehata TMA, Pelfort X, Monllau JC. Knee Autograft soaking in vancomycin reduces the risk of infection after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2724-8.
-
7Lind M, Nielsen T, Faunø P, Lund B, Christiansen SE. Free rehabilitation is safe after I solated meniscus repair: a prospective randomized trial comparing free with restricted rehabilitation regimens. Am J Sports Med. 2013;41(12):2753-8.
-
8Brown CA, McAdams TR, Harris AHS, Maffulli N, Safran MR. ACL reconstruction in patients aged 40 years and older: a systematic review and introduction of a new methodology score for ACL studies. Am J Sports Med. 2013;41(9):2181-90.
-
9Desai N, Björnsson H, Samuelsson K, Karlsson J, Forssblad M. Outcomes after ACL reconstruction with focus on older patients: Results from The Swedish National Anterior Cruciate Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2014;22(2):379-86.
-
10Cinque ME, Chahla J, Moatshe G, et al. Outcomes and Complication Rates After Primary Anterior Cruciate Ligament Reconstruction Are Similar in Younger and Older Patients. Orthop J Sports Med. 2017;5(10):1-6.
-
11Bedi A, Kawamura S, Ying L, Rodeo SA. Differences in tendon graft healing between the intra-articular and extra-articular ends of a bone tunnel. HSS J. 2009;5(1):51-7.
-
12Williams A. The Anterolateral Ligament: The Emperor’s New Clothes? Arthroscopy. 2018;34:1015-21.
-
13Marom N, Ouanezar H, Jahandar H, Zayyad ZA, Fraychineaud T, Hurwit D. Lateral Extra-articular Tenodesis Reduces Anterior Cruciate Ligament Graft Force and Anterior Tibial Translation in Response to Applied Pivoting and Anterior Drawer Loads. Am J Sports Med. 2020;48(13):3183-93.
-
14Devitt BM, Bell SW, Ardern CL, Hartwig T, Porter TJ, Feller JA. The role of lateral extra-articular tenodesis in primary anterior cruciate ligament reconstruction: a systematic review with meta-analysis and best-evidence synthesis. Orthop J Sport Med. 2017;5(10):1-12.
-
15Gómez Cáceres A, García-Germán Vázquez D, Espejo Reina A, López Rubia E, Tamimi Mariño I, Espejo Baena A. Revisión sistemática: ligamento anterolateral de la rodilla. Rev Esp Artrosc Cir Articul. 2018;25(1):56-70.
-
16García-Germán D, Menéndez P, González S, de la Cuadra P, Rodríguez-Arozena R. Extra-Articular Lateral Tenodesis for Anterior Cruciate Ligament Deficient Knee: A Case Report. Case Rep Orthop. 2013;2013:1-5.
-
17Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between Objective Assessment of Ligament Stability and Subjective Assessment of Symptoms and Function after Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2004;32(3):629-34.
-
18Zhu M, Han Lee DY, Williams A. Safe Femoral Fixation Depth and Orientation for Lateral Extra-Articular Tenodesis in Anterior Cruciate Ligament Reconstruction. Orthop J Sport Med. 2021;9(1):1-8.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- From the start to the top: the history of knee osteotomies
- Clinical-functional and radiographic outcomes of medial valgus-producing tibial osteotomy
- Patellar tendinopathy: a practical consensus guide for choosing the best treatment
- Evolution of spinal endoscopy. Where do we come from and where are we going?
- Partial ruptures of the rotator cuff
- Arthroscopic core decompression of the femoral head with autologous stem cell placement as treatment for femoral head osteonecrosis
- Extraarticular plasty as sole maneuver in the correction of rotational instability due to rupture of the anterior cruciate ligament in an elderly patient
- Fully arthroscopic osteosynthesis with button placement in acute anterior glenoid fracture: a case report
- Arthroscopic visualization of the popliteal hiatus and localization of an intraarticular free body
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.